Breast and chest lymphedema and swelling are common after breast cancer surgery or radiation. In this post, you will learn treatment options and ways to reduce swelling and lymphedema of the breast from a certified cancer and lymphedema physical therapist.
Swelling of the chest or breast is often a side effect of breast cancer surgery and radiation that is rarely spoken about, yet it affects many individuals. Sometimes the swelling is temporary and goes away once done healing, but for others, the swelling can be lymphedema, which can last long-term. Let’s explain the difference, who is most at risk for developing lymphedema of the breast, and how it’s treated.
👋 Hello, I’m Kelly Sturm, a Doctor of Physical Therapy (PT, DPT) and a Board-Certified Oncology Specialist, CLT-LANA. I share helpful resources for those living with and after breast cancer and lymphedema. Subscribe to my YouTube Channel, get my free guides, or learn more about my comprehensive program Breast Cancer Rehab.
What Causes Breast Lymphedema? Who is at Risk?
Surgery is one of the main treatment options for breast cancer and melanoma cancer in the upper body. Some individuals will have a mastectomy, where all breast tissue is removed. Others may have breast-conserving surgery, often called a lumpectomy, where only the tissue around the tumor is removed. With either of these surgeries, lymph nodes are biopsied or removed from the armpit, called the axilla.
There are two kinds. A sentinel lymph node biopsy is when 1-5 lymph nodes are removed to check if cancer has spread to the lymph nodes. An axillary lymph node dissection removes a more significant number of lymph nodes to further assess for disease or taken because cancer is present.
After surgery, there will be some level of swelling that occurs. It’s a normal response to surgery, and swelling can take 4-6 weeks to decrease. For some, it’ll be quicker, and for others, the swelling may linger for a few months. This type of swelling is called post-surgical swelling, and it usually is temporary.
Swelling that occurs long-term is often lymphedema of the breast. It’s common to hear about the risk of lymphedema in the arm after surgery, but often the breast lymphedema isn’t brought up or monitored as closely. So who is most at risk?
The primary risk factor for developing lymphedema in the arm or breast is the number of lymph nodes removed—the greater the number, like with an axillary lymph node dissection, the greater the risk. If someone had less than five lymph nodes removed, then the risk of getting lymphedema in the area is less than a 5% chance in someone’s life. If someone had eight or more lymph nodes, that number does increase to around 20% change.
Radiation therapy to the chest and breast also increases someone’s risk for lymphedema in the arm or breast. The risk of getting lymphedema in the breast and chest is much higher for those who had radiation compared to those who do not get radiation.
Radiation can cause radiation fibrosis in the area. Fibrosis is like scar tissue that damages the muscles and other tissues in the region. This fibrosis can thicken and scar lymphatic vessels and pathways, which leads to congestion and swelling. A cancer rehabilitation therapist can help minimize radiation fibrosis, but it is not entirely avoidable.
For both the arm and the breast, obesity and body mass index (or BMI) are other risk factors due to the potential of fatty tissue blocking or clogging the pathways. Those with denser breast tissue may also be at a higher risk for lymphedema.
So anyone who has lymph nodes removed or radiation therapy is at risk. Monitoring for any swelling is essential to address it as soon as possible.
How do you know if you have Breast Lymphedema?

What do you want to look for? Look for any breast fullness, skin texture changes, or peau d’orange, which means it looks like the peel of an orange with small dimpling. The breast or chest may be firm and full. Someone with swelling of the breast may explain that the breast feels heavy, aching, or painful. They may notice clothes or bras fit differently or tighter on that side. Swelling may even wrap around to the side of the chest and into the back. Some individuals will describe noticing that their arm doesn’t rest against the side.
To confirm that this swelling is lymphedema, it’s essential to ensure someone doesn’t have an infection. So if someone has swelling, pain, redness, or the breast is hot to touch, they should urgently reach out to a doctor or seek medical attention.
There may also be a pocket of swelling near the incision or surgical area after surgery. This can be what is called a seroma. This isn’t lymphedema, and some go away on their own or with light compression treatment, but if not, some are drained by the surgeon.
How to Treat or Reduce Breast Lymphedema
If cleared for any safety concerns, then there are treatment options. Some need to wait until all cancer treatment is done, and some don’t, so someone must work with his, her or their doctor and therapist for more guidance, but I am going to talk about the various treatment options here briefly.
There are four main treatment options to help reduce and manage breast lymphedema. Along with these, there are other ways and specific tools that someone can use to help them reduce swelling and pain.
→ You can find my favorite techniques and treatment for Breast Swelling and Lymphedema in my program Breast Cancer Rehab.
Lymphatic Drainage for the Breast
Lymphatic drainage is the primary treatment of lymphedema of the breast. Manual lymphatic drainage is a massage-like technique done in a specific sequence with a gentle method to move fluid out of a congested area to reduce the liquid. This will also help improve someone’s skin texture and help avoid infections. A certified lymphedema therapist can perform this, but it may be something you need to do long term, and learning how to do it yourself at home can be very beneficial.
Click Here to find a printable handout with easy-to-follow, step-by-step instructions for lymphatic drainage of the chest.
Or
You can follow along with me in a complete, step-by-step sequence here:
Compression for Breast Lymphedema
Compression is well-known as a form of treatment of swelling or lymphedema in the arms and legs. It’s used to support the chest in the same way. Giving comfortable compression to the chest and the areas of swelling can help reduce the volume or size and lower pain and aching.
The best compression option for breast lymphedema is a compression bra. Compression bras look like sports bras, but they are specifically for lymphedema. However, they are hard to find! My favorite compression bras are from Prairie Wear . Prairie Wear has a beautiful line of compression bras that come in an extensive range of sizes and the ability to adjust. They have removable cups, so they can be worn to shape for various sizes of breasts, or they can be removed, and the bra will lay flat for those who have had a mastectomy. They are high and wide on the sides of the chest for full coverage. This is important because these are common areas where lymphedema and swelling occur. The bras have adjustable straps and a smooth band without an underwire. The bras zip in the front, making them easier to get on and off, and an extender for size changes.
Update *Prairie Wear reached out with a code for you all! For 10% their website, use affiliate code CANCERREHABPT
Another tool for compression is L&R’s Swell spot. This padded insert goes inside a compression bra or tank to give extra compression. It has foam chips inside for a gentle way to soften the skin for any hardening or thickening from fibrosis, which occurs due to lymphedema and fluid sitting there too long, or radiation-induced fibrosis. They come in various shapes and sizes to fit what someone needs, but many individuals like the breast swell spot for the best coverage and fit to the area.
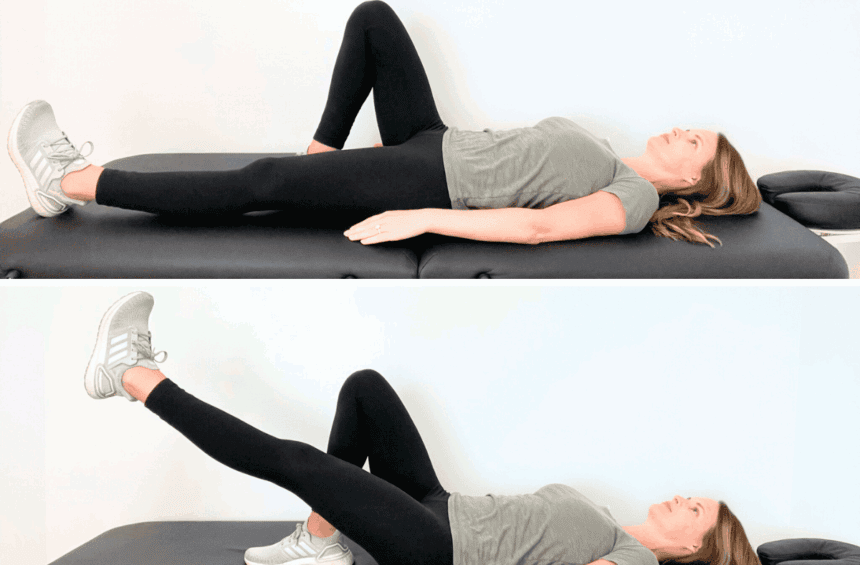
Exercise for Breast Lymphedema and Swelling
Exercise is another important treatment option for breast lymphedema. The muscles in the body act as a pump to the lymphatic system, and this can help work to move fluid out of a congested area. The movement around the lymphatic vessels helps propel fluid through small valves and guides along through the space towards your lymph nodes and then back to the heart. Exercise is best done with a compression bra to further help with lymphatic fluid movement and flow.
If you are looking for exercises, you can find various 10-20 minute exercise routines in a playlist HERE.
You can also follow along below with simple movements in a sequence for lymphedema drainage.
Deep Breathing for Breast and Chest Lymphedema
Lymphatic fluid moves from your body through vessels and eventually goes back to the heart. Many of those pathways and vessels are in the abdomen and lead to the upper chest and heart. The vessels and lymph nodes in the abdomen are deep, so lymphatic drainage to the skin isn’t adequate. Adding deep breathing or diaphragmatic breathing will stimulate the lymphatic system to keep fluid flowing and help avoid congestion or lymphedema. When breathing for lymphedema, it’s essential to focus on expanding the abdomen with the breath rather than the chest. Watch THIS video for guidance.
Other Treatment Options for Breast Lymphedema
Breast and chest lymphedema may also be treated with kinesiology tape, weight management, and avoiding infections. Kinesiotape is used on the skin to help lift the skin gently for lymphatic flow. A Youtube video is coming soon on this technique, so subscribe HERE to watch this video.
As mentioned earlier, maintaining a healthy weight can help lower the risk of getting lymphedema. Still, it can also improve the health and flow of the lymphatic system and may decrease congestion and swelling. Infections increase one’s risk of getting lymphedema, and they can also make lymphedema worse. So cleaning cuts and skin openings well and seeing a doctor urgently for any signs of infection is essential.
Chest, trunk, and breast lymphedema are challenging side effects of melanoma or breast cancer surgery and radiation. There are ways to reduce the swelling, but often lymphedema is chronic and will last long-term. Working with a cancer rehabilitation or certified lymphedema therapist early in cancer treatment can help screen for and treat signs of swelling as soon as possible and help reduce as much swelling as possible and guide for the best way for each individual to manage breast lymphedema.