If you’ve recently undergone cancer treatment or had your lymph nodes removed, you may be at an increased risk of lymphedema. Lymphedema is a chronic swelling in your arms, legs, or other affected areas.
As a Doctor of Physical Therapy and a Certified Lymphedema Therapist, I often get asked how to prevent lymphedema. The truth is, while lymphedema is common, it doesn’t have to become your new normal – even if you’re at a high risk of developing it.
In this article, I’ll share educational information about what lymphedema is and how to prevent it from developing so you can go on to live a healthy and fulfilling life.
What Is Lymphedema?
Lymphedema1 is a condition that develops when the lymphatic system, which is responsible for draining excess fluid from your body, becomes damaged or blocked. As a result, certain body parts begin to accumulate lymph fluid, causing swelling and discomfort. Lymphedema can affect any part of the body but is most commonly seen in the arms and legs.
Lymphedema often develops as a result of cancer treatment, particularly breast cancer treatment. However, sometimes people develop lymphedema for unknown reasons or because of genetic factors.
Lymphedema is a chronic condition with no known cure, but there are ways to manage it to reduce swelling effectively. In the early stages, you can even sometimes reverse lymphedema symptoms.
Your Lymphatic System
The lymphatic system is an important part of your immune and circulatory systems. It consists of lymph nodes, lymphatic vessels, and lymph fluid. The lymphatic system helps remove waste, toxins, and other unwanted materials from your body.
Your lymph nodes act as filters, trapping bacteria and viruses so that they can be destroyed by special white blood cells. When you have lymphedema, your lymphatic system doesn’t work properly. Lymphatic fluid gets trapped in certain body parts, making the affected area swollen and uncomfortable.
Primary Lymphedema
Primary lymphedema is a genetic condition caused by inherent malformations in the lymphatic system. Primary lymphedema can present at any age, from infancy to adulthood, and varies in severity. However, it’s extremely rare, only affecting 1 in 100,000 individuals2.
Secondary Lymphedema
Secondary lymphedema is the most common type of lymphedema, affecting approximately 1 in 1000 Americans. It develops as a result of damage or blockage in the lymphatic system after surgery, radiation therapy, infection, or trauma. It is often seen in cancer patients who have undergone lymph node removal or radiation treatment, which can negatively impact lymphatic drainage.
Risk Factors for Developing Lymphedema
Understanding the risk factors for lymphedema can help you take preventive measures. Educating yourself is one of the most powerful tools when it comes to preventing lymphedema.
Surgery
Surgeries that involve the removal of lymph nodes, such as sentinel lymph node biopsy, lymph node surgery, and other cancer-related surgeries, can disrupt lymphatic flow and increase your lymphedema risk.
Trauma from surgery can prevent your lymph fluid from draining naturally, leading to its accumulation in the affected arm, leg, or another area.
Radiation Therapy
Radiation therapy, often used in breast cancer treatment and other cancer treatments, can cause scarring and inflammation of lymph nodes and vessels. This damage can prevent proper lymphatic drainage and increase your risk of developing lymphedema. It can also result in other unwanted side effects, such as radiation fibrosis.
Infections
Infections can cause inflammation and damage to your lymphatic system, increasing your risk of lymphedema. Bacterial infections such as cellulitis can lead to swelling and compromise lymphatic function. If you develop an infection, it’s essential to treat it right away to lower your lymphedema risk.
Obesity
Excess weight can put additional pressure on your lymphatic system, negatively affecting its function and increasing the risk of lymphedema. Maintaining a healthy weight is one of the most important factors for your lymphatic health, so it’s essential to eat a healthy diet and regularly do low-impact exercise to lower your lymphedema risk.
Inactivity
Lack of physical activity can negatively impact lymphatic drainage. Regular movement and exercise help stimulate lymph flow and reduce the risk of fluid accumulation. If you tend to stay sedentary throughout the day, try to take breaks to move more often to proactively lower your risk of developing lymphoedema.
Genetics
A family history of lymphedema can increase the risk of developing the condition. Genetic predisposition can affect the development and function of your lymphatic system, making you more susceptible to lymphedema. In this case, breast cancer surgery or another risk factor can trigger lymphedema more easily.
That said, even if you have a genetic predisposition, you can learn how to successfully lower the risk of developing lymphedema.
Symptoms of Lymphedema
Lymphedema symptoms can vary in severity and often develop gradually. Common symptoms include:
- Swelling: Noticeable in the affected limb or area, often accompanied by a feeling of heaviness or tightness.
- Pain or Discomfort: Caused by the swelling and pressure on surrounding tissues.
- Restricted Range of Motion: Difficulty moving the affected limb due to swelling and stiffness (ex: it can be difficult to brush your hair).
- Skin Changes: Thickening, hardening, or development of fibrotic tissue in the skin.
If you notice any of these lymphedema symptoms, you should get in touch with your medical team and create a proactive lymphedema self-care routine to reduce symptoms and improve your quality of life.
Putting off lymphedema treatment can often make lymphedema worse. In turn, knowing what the early signs of lymphedema are and promptly acting on them can help you significantly reduce swelling and potentially even reverse it.
Stages of Lymphedema
Lymphedema is classified into different stages based on severity. The more severe lymphedema is, the more difficult it is to manage the symptoms. Early lymphedema treatment can help you prevent lymphedema from progressing.
Stage 0
In this stage, there is no visible swelling, but the lymphatic system has been damaged, and fluid accumulation may occur over time. You may experience a feeling of heaviness or discomfort in the affected area. At this stage, lymphedema is often reversible3.
Stage 1 (Mild)
This stage is characterized by mild swelling that may reduce when you elevate your arms or legs. The skin remains soft, and the swelling is generally reversible with proper management. Early intervention is crucial to prevent the progression of the condition.
I share early intervention resources in my programs Lower Body Lymphedema Rehab (for lower body lymphedema) and Breast Cancer Rehab (for lymphedema after breast cancer treatment).
Stage 2 (Moderate)
In this stage, lymphedema swelling is more persistent and uncomfortable. Your skin may begin to harden and fibrotic tissue may develop. Management becomes more complex, and you’ll need consistent treatment.
Stage 3 (Severe)
In stage 3, people experience severe swelling, skin changes, and significant fibrosis. The affected area becomes large and disfigured, with possible infections and complications. There’s a need for intensive treatment and management. With proper lymphedema treatment, many people can prevent reaching stage 3.
How to Prevent Lymphedema: Tips from a Certified Lymphedema Therapist
As a physical therapist and a Certified Lymphedema Therapist, I often work with people who have been told that they just have to accept discomfort and swelling as their new normal instead of being given helpful resources to prevent and treat lymphedema.
Lymphedema is a chronic condition, but there is a wide range of things you can do to prevent it from developing or getting worse.
1. Maintain a Healthy Weight
Maintaining a healthy weight reduces the strain on your lymphatic system and helps prevent lymphedema.
Focus on a balanced diet rich in fruits, vegetables, lean proteins, and whole grains. Avoid excessive salt, sugar, and unhealthy fats. Regular exercise can help manage weight and improve lymphatic function and the health of your immune system.
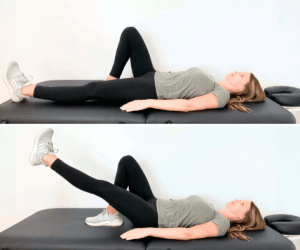
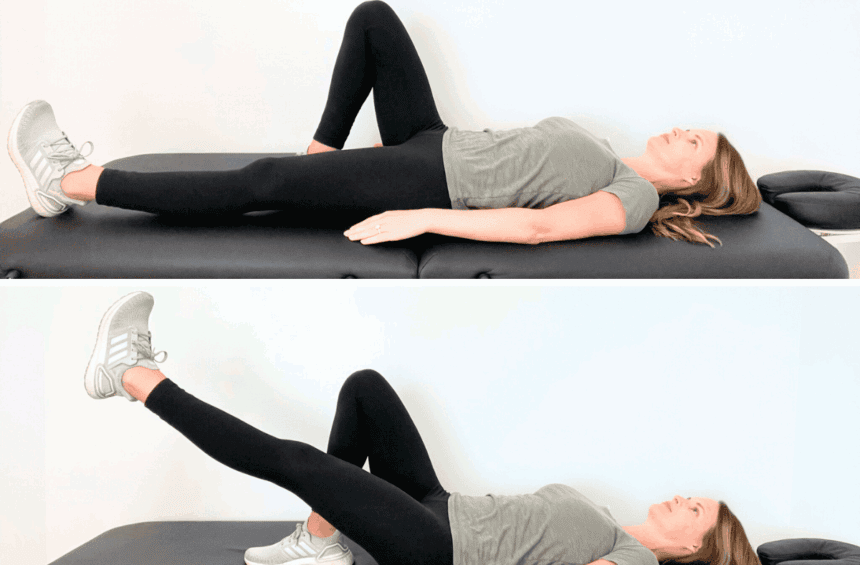
2. Stay Active
Physical activity can do wonders for your health and improve lymphatic drainage. For people with an increased risk of lymphedema, low-impact exercise such as walking, swimming, or cycling is best. You can also try yoga or tai chi to improve your lymph flow.
If you’re recovering from cancer or breast surgery and treatment, start slow with just a few minutes of exercise per day and gradually build up to 25-30 minutes of physical activity. It’s important to set realistic expectations and goals instead of pushing yourself too hard.
As a Doctor of Physical Therapy and a Certified Lymphedema Therapist, I’ve developed several exercise guides that you can print out and use to stay active:
- Exercises for Leg Swelling and Lymphedema
- Exercises for Arm and Chest Swelling and Lymphedema
- Leg Circulation Exercises
- Exercises for Abdominal and Trunk Swelling and Lymphedema
- Exercises for Head and Neck Swelling and Lymphedema
If you don’t know where to start with physical exercise for lymphedema prevention and want to use resources developed by a medical professional with extensive experience in treating lymphedema, these guides will be helpful!
3. Practice Good Skin Care
Skin infections can trigger lymphedema, especially when you’re recovering from cancer treatment or surgery.
Keep your skin clean and moisturized to prevent dryness and cracking. Avoid cuts, scrapes, and burns when going about your daily activities, such as cooking. When getting your nails done, don’t use sharp tools and try to file your nails instead of cutting them. If you get a cut or a skin injury, even if it’s small, care for it right away.
4. Don’t Wear Tight Clothing
When you wear tight clothing or accessories (such as bracelets), they can constrict lymphatic flow and increase the risk of swelling. Instead, try wearing loose-fitting, comfortable clothing that allows for proper circulation and lymphatic drainage.
For some people, this recommendation may come across as confusing because wearing compression garments is an effective and popular lymphedema treatment.
It’s important to know that compression therapy uses garments (such as a compression sleeve) that were specifically developed to treat lymphedema. You can wear special compression garments to manage swelling, but wearing regular restrictive clothing or accessories is not advisable.
5. Avoid Insect Bites
Insect bites can lead to infections and inflammation, increasing the risk of lymphedema.
Use insect repellent, wear protective clothing, and avoid outdoor activities when insects are active. Treat insect bites promptly with antiseptics to prevent complications, but don’t use harsh chemicals or soaps that can further irritate your skin.
6. Don’t Get Too Hot or Too Cold
Extreme temperatures can affect lymphatic function. Avoid hot tubs, saunas, or extremely cold environments if you are at a high risk for lymphedema. Dress appropriately for the weather and use protective measures, such as sunscreen in the sun and warm clothing in the cold, to protect and support your lymphatic system.
7. Educate Yourself
Understanding lymphedema and its risk factors is crucial for prevention. Stay informed about the condition and seek advice from your healthcare provider, if that option is available to you. Knowledge empowers you to take proactive measures to reduce your risk and manage symptoms effectively.
If you’re looking for more education and support, I share in-depth knowledge in my programs Lower Body Lymphedema Rehab and Breast Cancer Rehab.
How to Prevent Lymphedema After Mastectomy
After a mastectomy, the risk of developing lymphedema increases due to the removal of lymph nodes, which can disrupt normal lymphatic drainage. However, it’s possible to lower your risk and prevent lymphedema from developing after a mastectomy.
Wearing compression garments, such as sleeves, as recommended by your healthcare provider can also help support lymphatic drainage and prevent fluid buildup.
Regular exercise is one of the most effective ways to prevent lymphedema after a mastectomy. Gentle exercises, including range-of-motion activities and stretching, can improve lymphatic drainage and maintain your flexibility. Get started with these exercises:
- Early Exercises for Breast Cancer When Drains Are Still in Place
- Beginner Stretches for Breast Cancer Recovery
- Beginner Strength Exercises for Breast Cancer Recovery
- Intermediate Strength Exercises for Breast Cancer Recovery
- Advanced Stretches for Breast Cancer Recovery
- Beginner Stretches for Radiation Recovery
- Advanced Stretches for Radiation Recovery
For more in-depth support, learn more about Breast Cancer Rehab!
How to Prevent Lymphedema After Lymph Node Removal
Lymph node removal disrupts normal lymphatic flow and can trigger lymphedema. To minimize this risk, do gentle, post-surgery exercises to prevent fluid accumulation.
Preventing infections is also crucial in reducing the risk of lymphedema. Practice good hygiene and promptly treat any infections to prevent complications that may make lymphatic issues worse. Stay well-hydrated to maintain fluid balance in the body and eat a well-balanced diet to recover faster.
How to Prevent Lymphedema in Legs
To prevent lymphedema in legs, engage in activities that promote leg movement, such as walking or swimming. Regular exercise helps maintain muscle tone and encourages lymph flow.
You should also avoid standing or sitting for long periods of time and take breaks to move around if you have a sedentary job. Elevating your legs above heart level can also reduce swelling and promote lymphatic drainage. Learn more in Lower Body Lymphedema Rehab.
Treatment for Lymphedema
While prevention is key, if you develop lymphedema, there are different things you can do to minimize your symptoms and maximize your life.
In the early stages, some people can even reverse swelling in the affected area. Early intervention is key. If you spot early signs of lymphedema, start using treatment strategies as soon as possible.
- Compression Therapy: Using compression garments or bandages to reduce swelling and support lymphatic function. Compression helps prevent fluid buildup and encourages lymph flow. Browse recommended compression garments I love and trust.
- Manual Lymphatic Drainage: A specialized massage technique that encourages lymph flow. Read more about manual lymphatic drainage for lymphedema.
- Exercise: Specific exercises designed to promote lymphatic drainage and improve mobility. I share tailored exercise programs in Lower Body Lymphedema Rehab and Breast Cancer Rehab.
When managing lymphedema, it’s important to experiment with different forms of treatment to find the most effective routine for you. Life doesn’t stop when you have lymphedema, but even small changes can lead to big results.
FAQs
Is there any way to prevent lymphedema?
While it may not always be possible to prevent lymphedema entirely, taking proactive measures such as maintaining a healthy weight, staying active, practicing good skincare, and avoiding tight clothing can significantly reduce the risk. Early intervention and monitoring are crucial for managing symptoms effectively. In some cases, spotting early signs and promptly implementing a treatment plan can reverse swelling in the affected area entirely. Educating yourself and equipping yourself with the right tools is the best way to prevent lymphedema from developing.
What is the main cause of lymphedema?
Lymphedema is most often caused by damage to or blockage of the lymphatic system. This can happen because of surgery, radiation therapy, infections, or trauma. Lymphedema that develops as a result of damage to the lymphatic system is called secondary lymphedema. Some people are born with genetic factors that trigger the development of lymphedema. This type of lymphedema is known as primary lymphedema. Secondary lymphedema is much more common than primary lymphedema.
Does drinking more water help with lymphedema?
Yes, staying well-hydrated can support your lymphatic function and help prevent fluid accumulation. Proper hydration helps maintain fluid balance and supports your body’s natural detoxification processes. Some people may be scared of drinking water because they think that it’ll make the swelling and fluid retention worse, but it works the other way around!
Can you reverse lymphedema?
While there is no known cure for lymphedema, early detection and appropriate management can significantly reduce symptoms, prevent progression, and, in some cases, reverse swelling. If you spot early signs of lymphedema, such as swelling, restricted range of motion, pain, and skin changes, promptly start a targeted treatment routine to minimize lymphedema’s impact on your life.
Get More Support from a Certified Lymphedema Therapist
If you are at risk of or are already experiencing lymphedema, seeking support from a certified lymphedema therapist can be extremely helpful. Your therapist can help you develop a personalized treatment plan with exercises, compression therapy, and manual lymphatic drainage to help you reduce swelling and other symptoms.
However, many people don’t have access to a certified lymphedema therapist and proper care. This is why I created online, self-paced programs Lower Body Lymphedema Rehab and Breast Cancer Rehab. Inside, you’ll find the exact tools and exercises I use with my physical therapy clients adapted for the online format so you can reclaim control of your life and effectively prevent lymphedema.