Lymphedema is a chronic condition that causes swelling in different parts of the body, such as your arms and legs. Leg lymphedema is one of the most common types of lymphedema and it can impact your mobility, comfort, and overall quality of life. As a Certified Lymphedema Therapist (CLT-LANA), I often get asked how to prevent lymphedema in legs.
Even though it’s not always properly discussed, lymphedema often emerges as a consequence of cancer treatment. That said, there are other risk factors, such as genetic predispositions and lifestyle choices, that can trigger leg lymphedema.
If you’re at risk for leg lymphedema, it’s important to educate yourself on what you can do to prevent the condition from developing.
Building healthy habits and practices can drastically lower your risk and help reduce swelling you may have already started to develop. Let’s dive in!
What Is Leg Lymphedema?
Leg lymphedema is a chronic swelling in the legs that develops as a result of impaired lymphatic drainage. The lymphatic system is responsible for fluid balance and immune function, but it can be compromised by factors such as surgery, radiation therapy, infections, obesity, trauma, or genetic predispositions.
When the lymphatic system can’t efficiently remove excess fluid from the legs, fluid buildup accumulates and leads to swelling, discomfort, and reduced mobility.
Lymphedema is a chronic condition without a known cure, but lifestyle modifications and treatment can alleviate symptoms and greatly improve your quality of life. There are ways to make living with leg lymphedema more comfortable and minimize limitations.
Primary Lymphedema
Primary lymphedema is a rare, inherited condition characterized by abnormal development of the lymphatic system. It can manifest at birth or later in life and often affects the legs, but can occur in other parts of the body as well. Only about 6.5 percent1 of lymphedema cases are primary lymphedema.
Secondary Lymphedema
Secondary lymphedema is much more common than primary lymphedema. It occurs as a result of damage to the lymphatic system. This damage can be caused by factors such as surgery, radiation therapy, infections, obesity, trauma, or other medical conditions.
Understanding Risk Factors of Leg Lymphedema
Several factors can increase your risk for lymphedema and leg swelling. Here are some of the most common causes.
1. Surgery
Surgery is a significant risk factor for lymphedema in the legs, particularly when lymph nodes are surgically removed. Generally speaking, the higher the number of lymph nodes removed, the higher the risk of developing lymphedema. Procedures such as cancer surgery or vascular operations can disrupt the lymphatic system’s delicate balance, preventing proper fluid drainage and causing swelling in the legs.
2. Radiation Therapy
Radiation therapy is used in the treatment of various cancers and can unfortunately contribute to the development of lymphedema. While targeting cancer cells, radiation can also affect surrounding tissues and organs, including the lymphatic system. It may damage or scar lymph nodes and vessels, leading to fluid buildup and swelling in the affected area.
If you’ve undergone radiation therapy in the past, it’s important to be aware of your risk of developing lymphedema. It can manifest months or even years following treatment, but building healthy habits helps minimize your risk!
3. Infections
Chronic or recurrent infections, especially those affecting the lymphatic system, can cause inflammation and scarring, impacting your lymphatic function. Conditions such as cellulitis, bacterial infections, and skin infections can trigger inflammation and damage to the lymphatic system, increasing fluid buildup and causing leg swelling.
4. Genetics
Some people may have a genetic predisposition to lymphedema, which makes them more susceptible to developing the condition. If you have a family history of lymphedema or genetic conditions affecting the lymphatic system, such as Milroy disease, you may be at higher risk of developing leg lymphedema.
5. Obesity
Obesity is a significant risk factor for developing leg swelling and leg lymphedema. Excess body weight puts pressure on the lymphatic system, compromising its ability to drain fluid and leading to fluid buildup and swollen legs. Obesity can also increase inflammation, which makes swelling worse. People who are overweight or obese are at a higher risk of developing lymphedema in the legs.
6. Trauma
Injuries such as fractures, sprains, or surgical trauma can damage the lymphatic vessels and disrupt the flow of lymph fluid. If you have experienced trauma to the legs or had surgical procedures done in the legs, you may be at a higher risk of developing chronic leg swelling.
How to Prevent Lymphedema in Legs: 7 Strategies to Reduce Risk
Being at risk for developing leg swelling doesn’t mean that it will inevitably happen. There are lifestyle changes that you can make to lower your risk of lymphedema and live a fulfilling, swelling-free life.
As a Certified Lymphedema Therapist, I believe that prevention is the best treatment. Here are some of the things you can start doing to lower your risk of leg lymphedema!
1. Maintain a Healthy Weight
Maintaining a healthy weight is one of the most important things you can do to prevent leg lymphedema and swelling. If you’re at risk for developing lymphedema, your goal should be to maintain your lymphatic system as healthy as possible. Excess weight strains the lymphatic system, making it hard for it to effectively transport lymphatic fluid. As a result, fluid buildup can occur.
To lose or maintain a healthy weight, eat a well-balanced diet and engage in regular physical activity.
Weight loss is a long-term transformation, so it’s important to set manageable goals that you can stick to. Don’t restrict your eating with strict diets or try to exercise every single day. Instead, make small and sustainable changes for better overall progress.
2. Practice Proper Skin Care
You should keep your skin clean, moisturized, and free from cuts or injuries. Even minor cuts or tears can serve as entry points for bacteria, potentially leading to infection that can compromise your lymphatic system. Avoid bites and other injury.
You should also avoid harsh soaps or chemicals that can irritate your skin because inflammation can increase fluid buildup. When getting a pedicure, don’t use sharp tools, and try to file your nails instead of cutting them. Make sure the area between your toes is clean and dry. Avoid tight shoes and don’t walk barefoot to avoid getting an injury.
Overall, protect your skin from injury, skin infection, and irritation.
You can find more skin care tips in my YouTube video below!
3. Gradual Exercise
Regular physical activity helps promote lymphatic circulation and drainage, which is essential for maintaining healthy fluid balance in the body and preventing leg swelling. Walking, cycling, or swimming are great low-impact exercises that support lymphatic function in the lower limbs.
It’s important to incorporate exercises into your routine gradually and avoid overexerting yourself.
Especially if you’re still recovering from radiation therapy, hormone therapy, or other treatment, it’s crucial to go at your own pace and avoid putting too much pressure on yourself. Even 10-15 minutes of physical activity are beneficial.
If you don’t know where to start, try these lymphedema leg exercises or find more of them in my self-paced program Lower Body Lymphedema Rehab!
4. Avoid Prolonged Immobility
Avoid sitting or standing for long periods of time. Both activities can impede lymphatic flow and contribute to fluid buildup. When you’re sitting or standing for extended periods, gravity exerts pressure on your legs, ankles, and feet, hindering the upward movement of lymph fluid. This stagnant fluid can accumulate, leading to discomfort and leg swelling.
If you’re sitting at your desk for most of the day, try to take regular breaks to move and stretch.
You can try going on short walks or doing simple leg exercises to stimulate lymphatic circulation and prevent fluid buildup. You can also try elevating your legs a few times per day to encourage blood flow and ease swelling.
5. Don’t Wear Restrictive Clothing
Restrictive clothing, such as tight pants or clothing with seams and bands that dig deep into the skin, can constrict lymphatic flow and lead to fluid buildup.
❗It’s important to make the distinction between specialized lymphedema compression garments and restrictive clothing. Compression garments are an effective way to treat lymphedema, but restrictive or tight clothes can trigger swelling or exacerbate your symptoms. Compression garments and restrictive clothing are not the same thing.
Opt for loose-fitting clothing that allows for unrestricted movement and promotes healthy circulation.
Pants with a relaxed cut and an elastic waistband, flowy skirts, palazzo pants, or soft and stretchy leggings are all great options if you’re prone to leg swelling.
6. Be Mindful of Air Travel
There is not enough research on this, but traveling by plane may increase swelling. Flying typically involves prolonged standing or sitting, which can lead to fluid buildup in the legs.
This doesn’t mean that you have to avoid air travel at all costs. It simply means that you need to be mindful of the risks and take proactive measures. It’s possible that air travel won’t have any negative effects on you at all, but it’s a good idea to come prepared!
Stay hydrated by drinking plenty of water, avoid excessive alcohol and caffeine consumption, and move around periodically to promote circulation.
You can also try wearing compression garments or socks during flights.
7. Avoid Extreme Temperatures
Avoid being in overly hot or cold environments. Extreme heat can cause blood vessels to dilate and make your legs swell. In turn, extreme cold can cause blood vessels to constrict, reducing blood flow and leading to fluid buildup.
Avoid being outside in hot weather, stay hydrated, and seek shade or air-conditioned spaces when you’re starting to get overheated.
In cold weather, dress warmly to maintain adequate circulation in your leg veins and reduce swelling.
Recognizing Early Signs of Lymphedema and Leg Swelling
Recognizing early signs of lymphedema and leg swelling can help you take quick action and prevent mild swelling from getting worse. Watch out for persistent swelling, where the affected leg appears larger or feels heavier than usual. You may also experience discomfort or a feeling of heaviness in your legs. Decreased flexibility and a sensation of tightness in your skin can also be warning signs.
If you see any early signs of lymphedema or leg swelling, especially after radiation therapy or leg injury, monitor your symptoms and get in touch with your medical provider if they persist or worsen over time.
How to Treat Lymphedema and Reduce Leg Swelling
If you develop leg lymphedema, remember that it doesn’t mean that you have to accept swelling, discomfort, and pain as your new normal.
There are exercises and treatment practices that can help you control the swelling and alleviate lymphedema symptoms so you can live a fulfilling life with minimal restrictions.
If you’re starting to develop leg lymphedema, I encourage you to learn more about my program Lower Body Lymphedema Rehab. I combined everything I learned from over a decade as a Certified Lymphedema Therapist (CLT-LANA) in one comprehensive resource to help you effectively reduce swelling.

Compression Therapy for Leg Lymphedema
One of the best ways to treat leg lymphedema is using compression garments or stockings to put pressure on your legs and help move lymphatic fluid out of your ankles or legs to reduce swelling.
The standard treatment is to go through 2-5 weeks of compression bandaging with a certified lymphedema therapist. Then, once the inflammation goes down, you can start wearing compression stockings or garments as a part of your lymphedema self-care routine. You can learn more about compression therapy and choosing the right garments in my YouTube video below.
Physical Exercise
Regular physical exercise is a great way to lower your risk of lymphedema, but it’s also an effective form of treatment if you do develop leg swelling, whether it’s mild or severe swelling.
Staying active helps promote lymphatic circulation and drainage. Why? Because your muscles act as pumps for your lymphatic system, helping move fluid along and reduce swelling.
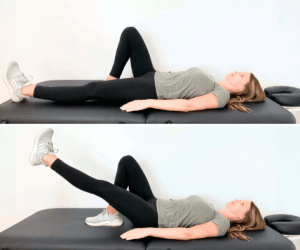
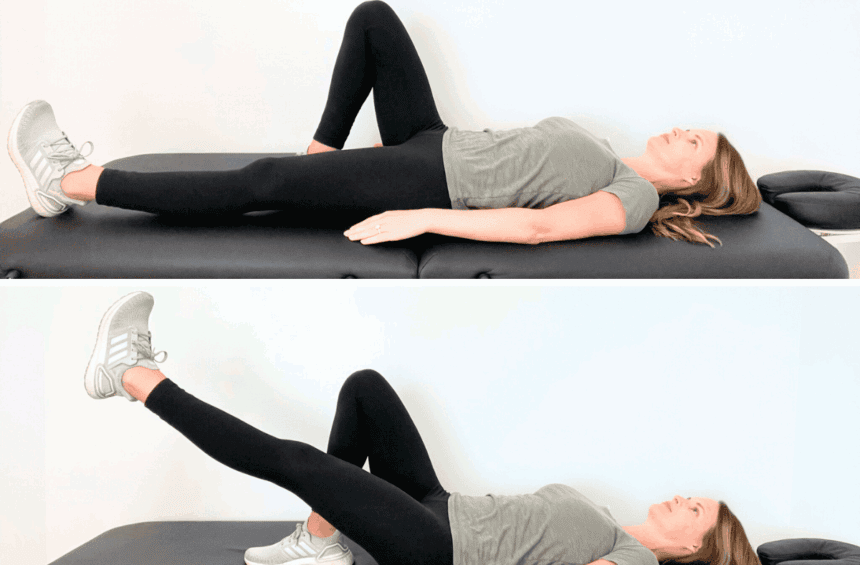
Bridges, leg raises, heel slides, and bicycle kicks are all great exercises to do if you have swollen legs. Here are a few exercises to help you get started!
Lymphatic Drainage Massage (MLD)
Lymphatic drainage massage (MLD) is a special technique that can help reduce swelling in the affected areas of your legs. You can do an MLD session with a trained therapist or try doing the massage at home. Lymphatic drainage massage involves gentle, rhythmic movements along your legs to encourage fluid circulation.
There have been new developments in lymphatic drainage research that have a great potential to help with lymphedema of the lower leg and body. You can watch my YouTube video to learn how to do lymphatic drainage massage for leg lymphedema.
Elevation for Leg Swelling
Elevation is a simple technique that can play a role in moving fluid out of the swollen area more efficiently. When you elevate your legs above heart level, gravity helps move lymph fluid out of the limb and reduce swelling.
You can prop up your legs on pillows or cushions while lying down or sitting or use a reclining chair. Try elevating your legs a few times per day for the best results. You can do it when you’re relaxing, watching TV, or taking a work break. Aim to elevate your legs for 15-30 minutes at a time.
Preventing Lymphedema in Legs FAQs
Can lymphedema be prevented?
While lymphedema can’t always be completely prevented, there are proactive measures you can take to reduce your risk of developing this condition. The first step is becoming aware of the risk factors and educating yourself on the steps you can take to support your lymphatic system and prevent swollen legs. Maintaining a healthy weight, preventing skin infection and injury, staying active, and avoiding prolonged standing are some of the ways you can minimize your risk of leg lymphedema.
What are the risks of lymphedema?
Several factors can increase your risk of developing leg lymphedema, including surgery, radiation therapy, being overweight or obese, having a skin infection, taking certain blood pressure medicines, undergoing hormone therapy, sitting or standing for long periods of time, recovering from surgery, and more. If you notice lymphedema symptoms starting to develop, get in touch with your medical provider.
What are the warning signs of lymphedema?
You may notice persistent swelling in your legs that doesn’t improve with elevation or rest, a feeling of heaviness or tightness, decreased flexibility or range of motion, and changes in the texture or appearance of your skin, such as thickening or hardening. You may also experience discomfort, pain, or a sensation of fullness in the swollen area, such as your ankles, feet, or legs.
Is walking good for leg lymphedema?
Yes, walking is a great way to prevent or treat leg lymphedema because it promotes lymphatic circulation and helps reduce swelling. Any low-impact exercise, such as walking, biking, or swimming, can be an effective way to lower your risk of developing lymphedema or alleviating the symptoms.
Can you cure leg lymphedema?
Lymphedema is a chronic disease with no known cure, but there are steps you can take to effectively manage it and reduce swelling. You don’t have to accept uncomfortable symptoms as your new normal. You can build a healthy self-management routine that makes you feel confident and in control. Learn more about Lower Body Lymphedema Rehab to get started 😊
Article Sources
- Mayo Clinic ↩︎