If you’ve recently had cancer surgery, you might notice a swollen area near your incision site. This condition is called a seroma, and it’s a fluid-filled pocket that forms under your skin.
Most small seromas are harmless and heal naturally, but a large one may require treatment. Here’s everything you need to know about a seroma after surgery so you can feel more confident and avoid any complications.
What Is a Seroma?
A seroma develops as a swollen area beneath your surgical site. It’s filled with clear fluid your body produces during healing. When you touch the area, it feels firm and may cause discomfort. Some seromas can be painful, especially if they’re large or pressing against nerve endings.
While it might look concerning, a seroma contains only clear fluid, not blood or pus. But it can slow down wound healing, increase the risk of infection, and cause discomfort.
Seromas often develop after breast cancer surgery, abdominal procedures, or any surgical procedures where a lot of tissue was removed and there’s now space under the skin as a result. They typically appear within the first few weeks after surgery, after the drainage tubes have been removed, near or around your incision site.
What Causes a Seroma After Surgery?
When you go through surgery, particularly cancer surgery, your surgeon often needs to remove tissue, which creates empty spaces or cavities in the area.
Your body naturally produces fluid as part of the healing process. But sometimes, this fluid collects in these empty spaces instead of being absorbed by surrounding tissues.
Postoperative seroma formation often happens after:
- Breast cancer surgery
- Abdominal wall surgeries
- Procedures where a lot of tissue was removed
- Any surgery that leaves a “dead space” that can fill up with fluid
According to one study, seroma formation is the most frequent complication after mastectomy and axillary surgery – it happens in up to 85% of cases. Another study found the risk to be as high as 51% after breast cancer surgery.
Seroma Risk Factors
Your risk of developing a seroma increases after surgeries where a lot of tissue is removed. These typically include breast cancer procedures, especially mastectomies.
The risk also goes up if the incision is in an area of your body that moves a lot during daily activities, such as your arms or chest.
The exact causes for why seromas develop are unknown, but here are a few factors that increase your risk:
- Having a large amount of tissue removed during your procedure
- Returning to activities too quickly after your operation
- Not wearing compression garments as recommended by your surgical team
- Lifting heavy objects or doing repetitive movements too soon after surgery
- Surgery in areas of your body that move frequently during daily activities
Your doctor will typically discuss specific risk factors for your procedure before the surgery. Make sure to follow their post-op instructions carefully.
Learn more about returning to exercise after a mastectomy.
Seroma Symptoms
The most common seroma sign is swelling or a visible lump near your surgical site. The swollen lump often feels firm when you touch it and may be tender or even painful to the touch, especially for large seromas. You might also see some redness where the fluid has collected.
Some swelling is normal after surgery. When the fluid build-up is due to a seroma, the swelling typically appears as a defined pocket of fluid rather than general swelling.
The skin around the seroma may sometimes look infected, but a seroma is not an infection – the color changes happen because of the fluid collection. Seroma is also not lymphedema.
Seroma Pictures After Breast Surgery
Here’s what a typical seroma at a surgical incision looks like.

How to Prevent Seroma Formation
You can’t fully prevent seromas, but there are things you can do to reduce your risk of developing one. Your surgical team will provide specific guidelines, but you should typically:
- Avoid lifting heavy objects or doing too much too soon after surgery. Even without heavy lifting, too much movement can increase fluid buildup.
- Limit yourself to gentle movements for the first 1-2 weeks of recovery.
- Wear proper compression garments once your surgical team approves them (typically 1-4 weeks after surgery). These garments should feel gentle and comfortable, not too tight.
- Stay well hydrated by drinking plenty of fluids throughout your recovery.
Overall, do your best to give your body the time and rest it needs to heal. This is one of the best things to do for postoperative seroma prevention.
You can learn more about minimizing your risk factors and building up your strength in Breast Cancer Rehab.
Seroma Treatment
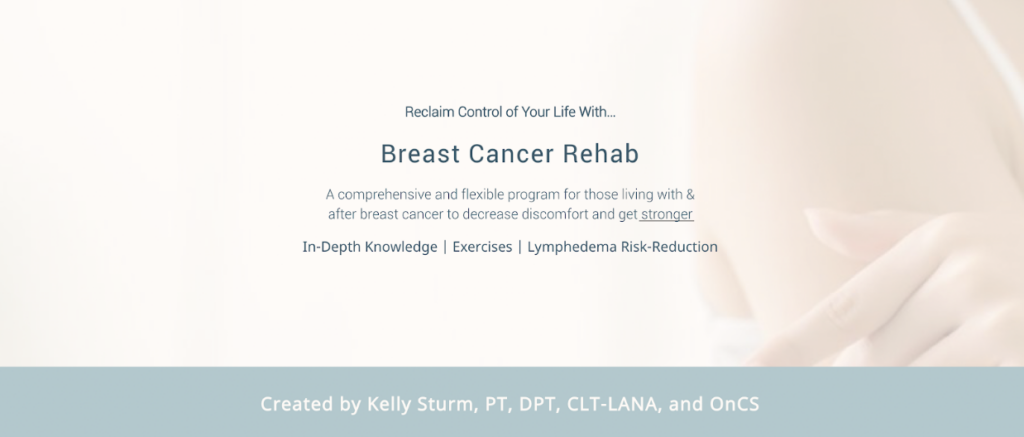
Not all seromas need treatment. Small seromas often naturally reabsorb or respond well to at-home management techniques like compression.
But if you have a large or chronic seroma, you might need surgical intervention and further treatment. In rare cases, a seroma can get infected, which requires immediate medical attention.
Small Seromas
Very small seromas often don’t need any special treatment. Your body can usually reabsorb the fluid naturally over time.
If you have a small but persistent seroma, gentle compression might help speed up the process. This could include wearing a compression bra or other compression garments that apply uniform pressure to the area.
You can also use swell spots and pads.

Browse my favorite breast cancer products for recommendations.
My favorite compression bra to help get rid of seromas is Prairie Wear’s HuggerPRIMA bra (use the code CANCERREHABPT for 10% off), which gives uniform, medical-grade full compression for swelling.
For added, gentle compression, I like to add in a compression pad like the L&R Lateral Bra SwellSpot or the JoviPak Slimeline Oval Pad (use the code CRPTKELLY for 10% off).
Large Seromas
Larger seromas typically need medical intervention. Your surgeon or doctor may need to drain the fluid using a needle and syringe, a process called seroma aspiration. It’s a minor surgical procedure.
Sometimes, seromas can refill after drainage. In this case, you’ll need multiple drainage procedures. After drainage, you can use compression to prevent the space from filling again while the area heals.
In severe cases, the seroma may have a cyst-like sac of tissue. If it’s bothersome or painful, it needs to be surgically removed, but if it doesn’t bother you, then it’s best to leave it alone to avoid further risk of infection with another surgery.

Seroma Warning Signs
Seromas typically aren’t dangerous, but they can sometimes become infected – especially larger ones. An infected seroma requires immediate medical attention, and you may need to take antibiotics or undergo another urgent treatment.
Watch out for these serious symptoms:
- Significant redness in the area
- Rapid onset of swelling
- Severe pain
- Fever
These symptoms might indicate an infection, blood clot, or other serious complications that need prompt medical treatment. Contact your doctor right away.
Seroma vs Lymphedema
Sometimes, it’s easy to confuse seroma for lymphedema and vice versa. But they are two different medical conditions.
Lymphedema is a chronic condition that causes swelling and discomfort in different parts of the body, most often in your legs or arms. It develops when your lymphatic system isn’t working properly, often after cancer treatments that affect your lymph nodes, such as surgery or radiation therapy.
Unlike seromas, lymphedema is a long-term condition that requires ongoing management.
A seroma is a temporary pocket of clear fluid that typically develops shortly after surgery near your incision site. The fluid in a seroma is different from lymphatic fluid, and seromas usually resolve on their own or with simple treatments like compression or drainage.
If you’re unsure whether you’re dealing with a seroma or lymphedema, make sure to reach out to your medical team. For lymphedema, seek out a Certified Lymphedema Therapist (CLT) for more support.
FAQs
How do you get rid of a seroma after surgery?
The treatment for a seroma depends on its size. Very small seromas often disappear on their own as your body naturally reabsorbs the fluid. For small but stubborn seromas, wearing compression garments and using specialized compression pads called swell spots can help speed up the process. Larger seromas typically need to be drained by your doctor using a needle and syringe. In some cases, multiple drainage procedures might be necessary if the seroma refills.
What happens if a seroma is left untreated?
An untreated seroma can sometimes lead to complications. Some small seromas may resolve on their own, but larger ones can become infected and require antibiotics. Over time, untreated seromas might develop a thick, fibrous capsule around them, becoming what doctors call a chronic seroma. These chronic seromas can cause ongoing discomfort and might eventually require surgical removal. Large untreated seromas can also make it more difficult for your incision to heal.
What do seromas look like?
A seroma typically looks like a swollen, raised area near your surgical site. The swelling usually forms a distinct bulge or lump under your skin that feels firm to the touch, kind of like a water balloon. You might also notice some mild redness in the area. The size can vary from a small bump to a larger swelling, depending on how much fluid has accumulated. Seromas often form in breast cancer patients after surgery, including a mastectomy, reconstructive surgery, and more.
How long does it take for seromas to go away?
It depends on the seroma’s size and the treatment. Small seromas might resolve on their own within a few weeks with proper compression and care. Medium-sized and large seromas that require drainage typically improve within several weeks to a couple of months, but you might need multiple drainage procedures.
Get More Support in Breast Cancer Rehab
Seroma after surgery is a common complication after a mastectomy, lumpectomy, breast reconstruction, and other procedures. Small seromas are typically left alone or managed with compression. Large and infected seromas require medical treatment.
Breast Cancer Rehab has in-depth education & physical therapy exercises that can help you improve your quality of life after cancer.