When you first receive the cancer diagnosis, your oncology team will walk you through what to expect during treatment. But many cancer survivors find themselves unprepared for what comes after that final treatment session and becoming officially cancer-free.
As a board-certified oncology clinical specialist and physical therapist with over 12 years of experience helping cancer survivors reclaim their strength, I’ve worked with hundreds of patients navigating life after treatment.
Having guided thousands of cancer survivors through their recovery journey, I’ve noticed a pattern: the transition from patient to survivor brings unexpected challenges that no one prepared them for. Here are the 5 things they never tell you about life after cancer, and I wish they did.
Life doesn’t just return to normal the day treatment ends, but knowing what to expect can help with physical rehabilitation and make you feel more in control.
What Are the 5 Things They Never Tell You About Life After Cancer?
1. It’s an emotional rollercoaster
It’s normal to experience different emotions after cancer treatment, both positive and negative.
Once you become cancer-free, you may feel that there’s an expectation that everything about your physical and mental health must be good, too. While you will feel happy about not having cancer anymore, the cancer rehabilitation process takes time.
It’s okay to not feel like your “old self.”
According to research, approximately 25% of cancer survivors experience some form of depression, a statistic I see reflected daily in my practice.
Many also feel anxious about cancer recurrence. You may feel like everything is different and struggle to maintain the same relationships or career.
In my experience, I often tell my patients that celebrating the end of treatment while simultaneously grieving the loss of their ‘old self’ isn’t contradictory. It’s human.
Everything you feel is valid.
So many of my patients tell me they wish someone had warned them about all of this. It’s common to feel the joy of completing treatment or achieving remission, but the anxiety about recurrence is less spoken about and can last for many years.
You may also feel a zest for life. Your perspective on things that truly matter might shift, and you may discover new passions or want to structure your daily life differently.
It’s essential to acknowledge all these emotions, but also to seek support and help when possible.
2. You may experience long-term fatigue
Fatigue is a common long-term side effect of cancer treatment.
Cancer-related fatigue isn’t the same as feeling tired after a long day. This type of fatigue doesn’t disappear after a good night’s sleep or a weekend of rest. Many survivors experience it for months or years after treatment.
One of my patients described it perfectly: “It’s like my battery only charges to 60% now.”
This resonates with so many individuals I work with. Some people describe feeling like they’re moving through thick fog or that their energy tank never fully refills.
If you experience fatigue, consider asking family and friends for help with tasks such as grocery shopping, cleaning, or other household responsibilities.
Light physical activity, even just a short walk, often helps more than complete rest, so try to incorporate regular physical activity into your daily routine, even if it’s just for 15 minutes.
It’s important to rest, but resting too much (for example, taking very long naps) can end up making you feel more tired and disrupt your sleep cycle. Experiment with different routines, and see if certain things improve your energy levels more than others.
Important note: If fatigue interferes with basic daily activities for more than 2-3 weeks, this warrants medical evaluation and discussion with your healthcare team.
3. There is a higher risk of lymphedema
If your cancer treatment involved removing lymph nodes or radiation to areas where lymph nodes are located, you’re at a higher risk of developing lymphedema.
Lymphedema is a chronic condition that causes swelling, usually in an arm or leg, because your lymphatic system can no longer drain fluid as effectively as before.
Symptoms of lymphedema include:
- Swelling in your arm, leg, fingers, or toes that doesn’t go down
- Feeling of heaviness or fullness in the affected area
- Skin that feels tight or stretched
- Decreased flexibility in your joints
- Clothes, shoes, or jewelry that suddenly feel too tight on one side
- Aching or discomfort in the affected limb
- Skin that looks thicker or feels harder than usual
Research shows that about 1 in 5 breast cancer survivors will develop lymphedema of the arm after cancer treatment. However, even though it’s so common, many cancer patients have never heard of lymphedema until they develop symptoms.
Early in my career, I watched too many patients develop advanced lymphedema simply because no one told them what to watch for. This is why education, bringing awareness, and early intervention have become so important in my work.
When you’re aware of the risk, you can take steps to proactively prevent lymphedema and reduce your risk of developing swelling.
Staying active is one of the best ways to support your lymphatic system because movement helps to naturally pump lymph fluid through your body. Swimming, walking, and gentle strength training are all great options. You can also try rebounder workouts.
If you notice any swelling or changes in how your arm or leg feels, don’t wait to see if it goes away on its own. Early treatment of lymphedema is much more effective than trying to manage it after it becomes severe.

4. Scar tissue will take time to heal
Scar tissue is a normal part of the surgery recovery process. However, it’s naturally denser and less flexible than normal skin.
You might notice tightness, pulling sensations, or restricted movement in areas where you had surgery, even months or years after. Scar tissue pain after a mastectomy is common.
What I consistently observe in my clinic is that patients who are proactive about scar tissue management have significantly better long-term outcomes.
You don’t have to accept that pain and limitations are a normal part of living after cancer. There are ways to improve these symptoms.
Here are my top recommendations for managing scar tissue:
- Keep it clean: Gently wash the area with mild soap and water daily, avoiding harsh scrubbing that could irritate the healing tissue.
- Moisturize: Apply a fragrance-free moisturizer or vitamin E oil daily using gentle circular motions to improve the scar’s texture and flexibility.
- Do scar tissue massage: Gently pick up and roll the scar tissue between your fingers to help break down adhesions and soften the area (check with your doctor first).
- Use sunscreen: Apply SPF 30 or higher to healed scars when exposed to the sun, as scar tissue is more prone to discoloration and damage.
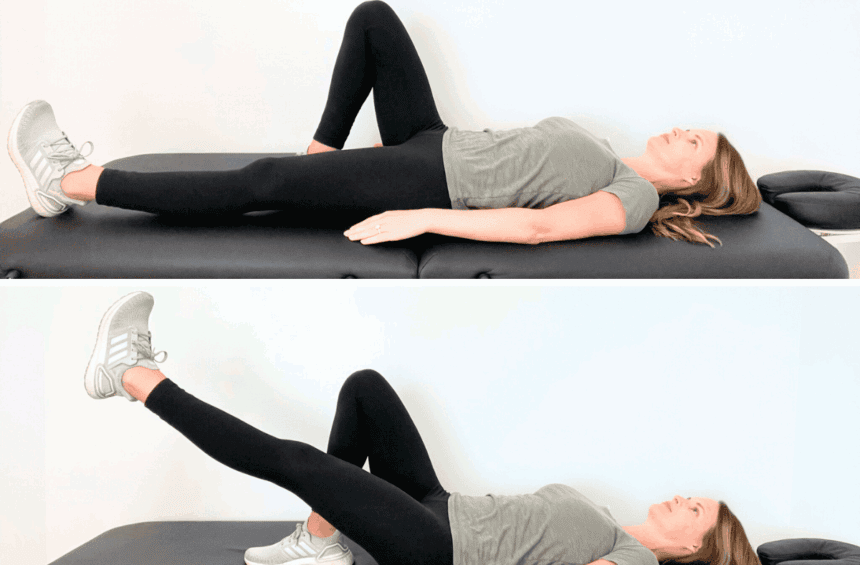
- Try active stretching: Do gentle stretching exercises targeting your chest, shoulders, and arms to prevent stiffness and improve range of motion around the surgical site.
You can find more education & exercises on managing scar tissue discomfort after cancer treatment in my program, Breast Cancer Rehab.
5. You may experience problems with sexuality and/or fertility
Medical teams typically focus on treating cancer and managing immediate side effects, and they don’t always discuss how treatment might affect your intimate relationships or plans for having children. However, these topics become important parts of your recovery and long-term quality of life.
Fertility concerns
Cancer treatments can impact your ability to have children, depending on the type and location of your treatment. Chemotherapy drugs and radiation therapy directed at your pelvis or abdomen can affect reproductive organs and hormone production.
Some fertility changes are temporary and improve as your body recovers from treatment. Others may be permanent. If you’re planning to have children in the future, discuss fertility preservation options with your oncology team before treatment begins.
Sexuality
Physical and emotional intimacy often changes after cancer treatment. Your relationship with your body may feel different, especially if you’ve had physical changes like surgical scars or hair loss. You might feel self-conscious or worry about how your partner perceives these changes.
Hormonal changes, fatigue, pain, and medication side effects can also impact your interest in sex or your body’s physical responses.
These changes don’t mean your intimate relationships are over, but they may require open communication and patience as you and your partner adjust.
In my practice, some people feel that discussing sexual concerns seems trivial compared to surviving cancer, but your intimate relationships and sexual health are important parts of your overall well-being and quality of life. So, don’t be afraid to bring up these concerns with your medical team or get help from a specialist.
Are You Ever the Same After Cancer?
Everyone’s cancer experience is different. What remains true for most people is that cancer creates big changes that touch almost every area of your life.
The physical side effects, such as fatigue and scar tissue pain, can persist long after treatment ends. If you had your lymph nodes removed during treatment, you may also be at a higher risk of developing a chronic condition called lymphedema.
However, physical therapy can help lower your chances of developing lymphedema and improve other physical challenges.
Emotionally, you may find that your priorities have shifted or that you approach life differently than you did before your diagnosis. You may not feel like the same person you were before, but different doesn’t mean worse.

You Have Agency Over Your Life After Cancer
Cancer can make you feel out of control. But as you move into recovery, you can begin to reclaim agency over your life.
Physical therapy and staying active can help you feel stronger and more confident in your body. Educating yourself on what to expect during recovery is empowering, too.
I always recommend discussing these concerns with your entire care team – your oncologist, primary care physician, and other specialists. As a physical therapist, I work closely with these providers to ensure comprehensive care and open communication.
When you understand what to expect with fatigue, lymphedema risk, or emotional changes, you’re better equipped to manage them.
Knowledge helps you make informed decisions about your care and gives you the tools to advocate for yourself with your healthcare team.
While I specialize in the physical aspects of cancer recovery, emotional and psychological support often requires additional professionals like counselors or even support groups, and that’s perfectly normal.
I share a lot of information on my YouTube channel that you may find helpful.
Tips for Physical Recovery
Stay active
Physical therapy and regular movement are very important during cancer recovery.
They help decrease fatigue and reduce your risk of developing lymphedema. Staying active also improves your mood and can help prevent scar tissue from becoming overly tight or restrictive.
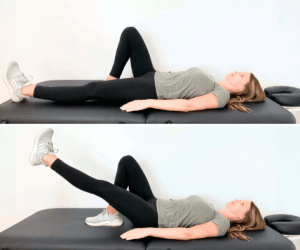
You don’t need to do intense workouts. Gentle activities like walking, swimming, or stretching are very beneficial, and you can also try following one of my physical therapy exercise guides:
I recommend that my physical therapy patients find a form of exercise that feels good to them, because then there’s a higher chance that they’ll do it consistently. Moving for 15 minutes every day is better than moving for 1 hour once a week.
Get enough sleep
Some people find it hard to sleep well after cancer treatment. It’s possible to sleep too little (sometimes, because of anxiety) or too much because of fatigue, which can often end up making you feel more tired.
Aim for 7-8 hours of sleep each night and try to maintain a consistent sleep schedule, going to bed and waking up at the same times daily.
If you take naps, try to keep them short and do it before 3 PM so that napping doesn’t interfere with nighttime sleep.
If you have trouble falling asleep, it can be helpful to create a wind-down routine before bed to signal to your body that it’s time to rest. This might include reading, gentle stretching, or listening to calming music. Keep your bedroom cool, dark, and quiet.
Build a manageable self-care routine
Make sure to pace yourself. It’s important to build a self-care routine after cancer, but it should be something you can stick to long-term.
Your physical activity and practices should fit realistically into your new life and energy levels.
Don’t force yourself to do activities you dislike just because they’re considered healthy. If you hate yoga but enjoy dancing, choose dancing. The best self-care activities are also ones that bring you joy and emotional satisfaction, too.
Living After Cancer Treatment Ends
Recovery from cancer isn’t a straight line. It’s natural to question your life, your relationships, and your priorities after such a significant experience. For some people, it’s helpful to seek emotional support from cognitive behavioral therapy, talk therapy, or support groups.
You may also experience physical challenges, but many of them can be improved with physical therapy.
If you’re at risk for developing lymphedema, taking proactive steps can also significantly lower your chances of developing this condition. Staying active can improve your emotional well-being, too.
Get Support in Breast Cancer Rehab
In my practice as a physical therapist & a board-certified oncology clinical specialist, I’ve seen many people who weren’t properly educated and supported through life after cancer.
This is why I created Breast Cancer Rehab, an online physical therapy program to minimize discomfort, build up strength, and improve your quality of life after treatment.
You’ll find education & exercises for:
- Breast Cancer-Related Arm Lymphedema
- Axillary Web Syndrome (Cording)
- Arm Mobility
- Breast Swelling/Lymphedema
- Scar Tissue
- Rehab After Radiation
If you have developed shoulder pain as a result of cancer treatment, you may also find my Healthy Shoulder Program helpful. For swelling of the lower body that may develop after cancer, check out Lower Body Lymphedema Rehab.