If you notice swelling in your arms, chest, or other parts of your body after breast cancer treatment, you may be starting to develop lymphedema. Lymphedema is a chronic condition characterized by lymph fluid buildup that leads to swelling and discomfort in affected areas.
Lymphedema after breast cancer is common, but you don’t have to accept limitations as your new normal. There are ways to effectively manage swelling and prevent it from becoming severe.
If you’re at risk of developing lymphedema after breast cancer treatment or have already started to notice swelling, here’s everything you need to know about supporting your lymphatic system.
What Is Lymphedema?
Lymphedema is a condition that occurs when there’s a blockage or damage to the lymphatic system. This damage or blockage leads to the accumulation of lymph fluid in the tissues, which causes swelling, pain, and discomfort in the affected area, such as your arm or chest.
Lymphedema is a chronic condition, but there are effective management strategies that can help you minimize limitations and live a healthy life.
There are two types of lymphedema, primary and secondary. Primary lymphedema is rare and refers to swelling due to inherent abnormalities in the lymphatic system. In other words, it’s something you’re born with. Secondary lymphedema develops as a result of a medical procedure or trauma, such as breast cancer surgery, radiation therapy, or infection.
Secondary lymphedema is much more common than primary lymphedema, affecting approximately 1 in 1000 Americans1.

Lymphedema after Breast Cancer Treatment
Breast cancer treatment commonly involves surgery, radiation therapy, and chemotherapy, all of which can affect the lymphatic system and increase your risk of developing lymphedema.
Surgery, particularly lymph node removal and sentinel node biopsy, disrupts the natural flow of your lymph fluid. Radiation therapy can cause scarring and inflammation in the lymphatic vessels, further impacting lymph drainage. Chemotherapy may also contribute to lymphedema by weakening your immune system.
Who’s at Risk for Lymphedema after Breast Cancer?
Lymphedema after breast cancer treatment is, unfortunately, common. Research shows that about 1 in 5 people (20%) will have lymphedema of the arm after breast cancer treatment 2that includes surgery to remove lymph nodes or radiotherapy to the lymph nodes.
You’re at risk of lymphedema after breast cancer treatment if:
- You had a breast cancer surgery, especially if it involved axillary lymph nodes, lymph node removal, axillary lymph node dissection, or sentinel lymph node biopsy
- You received radiation therapy to your chest or underarm area
- You had a high number of lymph nodes removed during breast surgery or had a large tumor
- You have risk factors such as obesity, older age, and pre-existing lymphatic conditions
Many breast cancer survivors are at risk of lymphedema, but it doesn’t mean that you will get cancer-related lymphedema.
There are things you can do to lower your lymphedema risk. If you’ve already started developing swelling, there are exercises and tools you can use to manage lymphedema symptoms and minimize limitations.
Symptoms of Lymphedema
Lymphedema after breast cancer can manifest with various symptoms. You should watch out for the following lymphedema symptoms:
- Swelling in the arm, hand, fingers, or chest on the side where surgery or radiation therapy was performed
- Feeling of heaviness, tightness, or discomfort in the affected arm
- Limited range of motion in the arm or shoulder that makes everyday tasks challenging
- Aching or pain in the affected area that may worsen with activity
- Recurring infections in the affected area
- Changes in the texture or appearance of the skin, such as thickening or hardening
- Swelling that worsens over time or does not improve with elevation or rest
- Visible differences in the size or shape of the arms or chest, compared to the unaffected side
Recognizing these symptoms early and contacting your healthcare provider can help you manage lymphedema effectively and prevent complications. Left untreated, lymphedema can result in more severe swelling and infections.
How Do You Diagnose Lymphedema?
Diagnosing lymphedema typically involves a physical examination, medical history review, and sometimes imaging tests such as lymphoscintigraphy or MRI. Early detection is crucial for effective management and preventing complications. If you’ve started noticing symptoms of lymphedema after being treated for breast cancer, get in touch with your doctor as soon as you can.
Lymphedema Treatment
While lymphedema is a chronic condition with no known cure, there are various steps you can take to stimulate your lymph flow and relieve symptoms of lymphedema.
Inside my program Breast Cancer Rehab, I have extensive resources on lowering your risk of breast cancer-related arm lymphedema and managing lymphedema symptoms like breast swelling.
1. Education and Awareness
The first step to successfully managing lymphedema after breast cancer treatment is educating yourself about the condition. When you are well-informed, you can make better decisions about preventive measures and lifestyle modifications to treat lymphedema, control swelling, and prevent infection. Educating yourself helps you feel more empowered.
Learning about lymphedema also helps you detect lymphedema symptoms early on and minimize the severity of the condition.
When you’re informed, you’re also better equipped to communicate with your healthcare providers, ask questions, and advocate for your health needs.
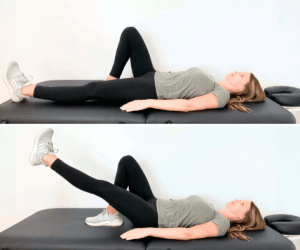
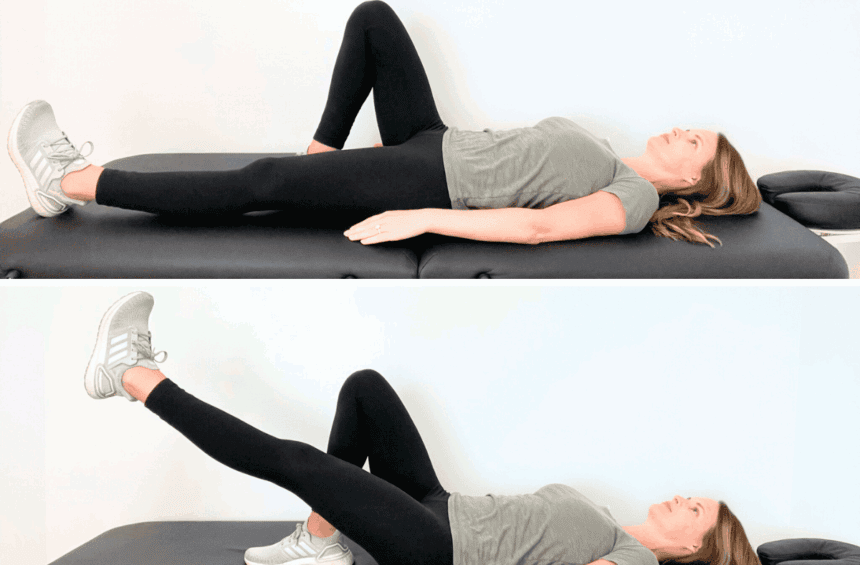
2. Exercise
Physical exercise plays a crucial role in lymphedema management and offers numerous physical and psychological benefits. As a Certified Lymphedema Therapist, I’ve seen firsthand the amazing benefits that engaging in regular and gentle exercise can have for people living with chronic lymphedema.
Exercise helps promote lymphatic flow, reduce swelling, and improve your overall mobility and flexibility.
Try activities such as walking, swimming, yoga, and tai chi because they encourage gentle movement without putting excessive strain on your affected arm, chest, or neck area. As a physical therapist, I also have several resources on exercises that you can do after breast cancer treatment:
- Early Exercises for Breast Cancer When Drains Are Still in Place
- Beginner Stretches for Breast Cancer Recovery
- Advanced Stretches for Breast Cancer Recovery
- Beginner Stretches for Radiation Recovery
- Advanced Stretches for Radiation Recovery
- Beginner Strength Exercises for Breast Cancer Recovery
- Intermediate Strength Exercises for Breast Cancer Recovery
- Advanced Strength Exercises for Breast Cancer Recovery
Beyond the physical benefits, exercise also improves your mental well-being and reduces stress and anxiety, which are common after surgical procedures and breast cancer treatment. Before starting a new exercise program, make sure to get cleared by your healthcare provider and build up the intensity of your exercises gradually.
3. Compression Therapy
Compression therapy is the practice of wearing compression garments, such as sleeves, gloves, and neck pads, that apply gentle pressure to the area of your body affected by lymphedema (ex: your arm).
Compression garments help reduce swelling, prevent fluid buildup, and improve circulation.
Compression therapy can help minimize discomfort and enhance your mobility. If you’re looking for a compression sleeve or other compression garments, here are some recommended products I trust and love!

4. Manual Lymphatic Drainage (MLD)
Manual lymphatic drainage (MLD) is a special massage technique that stimulates lymphatic flow and reduces swelling. It is a gentle and rhythmic massage that redirects lymph fluid toward healthy lymphatic pathways, helping with efficient drainage and waste removal from the body.
MLD can reduce swelling, alleviate discomfort, improve range of motion, and enhance your overall well-being.
Certified lymphedema therapists perform MLD sessions tailored to your specific needs and condition, but you can also learn how to do manual lymph drainage at home. I have several videos on my YouTube channel sharing lymphatic drainage routines and printable guides.
5. Skin Care
Proper skin care when living with lymphedema helps prevent skin infections and minimize complications associated with the condition.
When building your lymphedema self-care routine, focus on the following skin care habits:
- Keep your skin clean and gently wash it with mild, fragrance-free soap and lukewarm water
- Moisturize your skin regularly with hypoallergenic, non-irritating moisturizers to prevent dryness and cracking
- Wear sunscreen with a high SPF and stay in the shade when outdoors
- Avoid harsh chemicals, perfumes, and alcohol-based products that can irritate your skin
- Inspect your skin regularly for signs of skin infection, such as redness, swelling, warmth, or unusual changes
- Protect your skin from cuts, scratches, or insect bites by wearing protective clothing and gloves when gardening or performing other activities
- Use caution when shaving to avoid nicks and cuts, consider opting for electric razors or depilatory creams instead of traditional razors
- Keep your nails trimmed and clean to reduce the risk of infection
- Maintain a healthy diet and stay hydrated to support your overall skin health and immune function.
You should also focus on healing your skin after breast cancer treatment, especially if you went through radiation therapy. I have a YouTube video to help you get started!
6. Diet and Nutrition
A healthy diet and nutrition help you support your body’s natural healing processes and can minimize the severity of lymphedema.
Eat a balanced diet rich in fruits, vegetables, lean proteins, and whole grains for optimal immune function and tissue repair.
Remember to stay hydrated by drinking plenty of water throughout the day because proper hydration helps maintain lymphatic circulation and prevents fluid retention.
7. Psychological Support
Living with lymphedema often comes with a range of emotions, including stress, anxiety, frustration, and sadness, as you navigate the challenges of managing symptoms, especially after breast cancer treatment. Focus on supporting your emotional and mental well-being as you adjust to life with a chronic health condition.
Counseling, support groups, and peer networks can be great places to find encouragement, coping strategies, and a sense of community. When you share your experiences, concerns, and resources with others who understand your journey, you can feel more comfortable and validated by the fact that you’re not alone.
Most importantly, remember that knowledge is power.
Learning about lymphedema treatment can help you feel more in control of your symptoms and develop supportive routines that help you minimize swelling and discomfort.
It’s possible to live life fully after breast cancer – even if you’re starting to develop lymphedema. There are steps you can take to minimize symptoms, build up strength, and get your life back. I share effective tools & routines in my program Breast Cancer Rehab (including lymphedema therapy!).
How to Prevent Lymphedema after Breast Cancer Treatment
The 5-year survival rate for breast cancer is 90%. For many women, experiencing breast cancer is ultimately about creating a high quality of life after treatment. Lymphedema occurs in up to 40% of women treated for breast cancer3, but there are proactive steps you can take to reduce your risk and promote a healthy recovery.
1. Healthy Lifestyle and Weight Management
Adopting healthy habits can reduce your risk of lymphedema after treatment for breast cancer. You should focus on various aspects of your daily life, including diet, skincare, and stress management.
Obesity or morbid obesity is correlated with a higher risk of lymphedema, so it’s important to maintain a healthy body weight.
Eat a balanced diet of fruits, vegetables, lean proteins, and whole grains to support your overall health and stay at a healthy weight. Stay hydrated throughout the day for better lymphatic circulation. Practice regular skincare and keep your skin clean and moisturized. Get enough sleep and do your best to keep your stress levels low.
After breast cancer treatment, many women feel anxious about cancer recurrence or deal with unpleasant treatment side effects. In Breast Cancer Rehab, I share education and tips on how to successfully manage common concerns such as axillary cording, arm trouble bending after surgery, scar tissue, and more.
2. Physical Exercise
Engaging in regular exercise after breast cancer surgery can help you reduce the risk of lymphedema. Do gentle exercises that promote lymphatic circulation and improve overall mobility and flexibility. Physical activity also helps you maintain a healthy body weight, which is crucial for lymphedema prevention.
Try walking, swimming, yoga, or the physical therapy exercises on my YouTube channel.
Remember not to do too much too fast! Gradually increase the intensity of your workouts as you recover and gain more strength.
3. Avoid Infections
Infections can cause swelling, compromise lymphatic function, and trigger lymphedema.
Keep your skin clean, moisturized, and protected from cuts, scratches, insect bites, or skin sores to prevent infections.
Avoid harsh chemicals in your skincare routine and use a mild, fragrance-free soap. Wear gloves if you’re gardening, use sunscreen when a high SPF when you’re outside, and, in general, keep your skin protected. Leading a healthy lifestyle can also help your body fight infection if you develop one!
4. Don’t Wear Tight Bras or Clothing
Tight clothing, including bras with underwire or constrictive bands, can restrict the movement of lymph fluid and lead to fluid buildup, increasing your risk of lymphedema. Opt for well-fitted, supportive bras without underwires, and avoid tight clothing that compresses your chest or arms.
Choose breathable, non-restrictive fabrics that allow for freedom of movement and airflow.
This may sound confusing because earlier in this article, I discussed compression therapy (the practice of wearing compression garments) as one of the ways to treat lymphedema. It’s important to understand that not all pressure is good pressure. Compression garments are specifically designed to help reduce swelling and support your lymphatic system. Tight clothing and bras are not designed in the same way.
5. Early Detection
Lymphedema is a chronic disease that doesn’t have a cure, but catching it early and treating it right away helps minimize swelling and keep it from getting worse. In some cases, early detection can even reverse the swelling and make it go away completely.
You can do routine screenings at your hospital or clinic to detect lymphedema development, but it’s also important to know early signs of swelling and look for them yourself. Watch out for a sudden increase in size, heaviness, or discomfort in your arms, chest, neck, or other areas.
FAQs
How long after breast cancer can you get lymphedema?
Lymphedema can develop at any time after breast cancer treatment, ranging from weeks to years post-treatment. Unfortunately, the risk of developing lymphedema remains present for the rest of your life, particularly if you have undergone lymph node removal or radiation therapy as part of your breast cancer treatment. However, a healthy lifestyle, regular exercise, and certain lifestyle modifications can help you lower your risk of lymphedema. I share lots of resources and information in my program Breast Cancer Rehab!
How to prevent lymphedema after breast cancer?
You can take proactive measures to minimize your risk of developing lymphedema. First and foremost, it’s essential to educate yourself about the condition and its risk factors so you can recognize symptoms early and know exactly what to do about them. You should also adopt healthy habits, such as eating a well-balanced diet, staying hydrated, and taking good care of your skin. Regular low-impact exercise, such as walking, swimming, or yoga, can also help you stay healthy.
How can you tell if you are getting lymphedema?
After breast cancer treatment, you should pay close attention to changes in your body, particularly in your arms and chest area. Symptoms of lymphedema may include swelling, heaviness, discomfort in the affected limb, limited range of motion, recurring infections, changes in skin texture or appearance, and visible differences in size or shape compared to the unaffected side. Monitor for any gradual or sudden changes and get in touch with your medical provider if you notice any warning signs.
What exercises prevent lymphedema after breast cancer?
You should focus on exercises that promote lymphatic circulation and muscle strength while minimizing the risk of strain or injury. Gentle and low-impact activities such as walking, swimming, cycling, and yoga are great choices. You should also consider incorporating upper body exercises with light weights or resistance bands to strengthen the muscles and promote lymphatic drainage. I share extensive exercise routines in my program Breast Cancer Rehab!
How common is lymphedema after breast cancer?
Lymphedema is a relatively common complication after breast cancer treatment, with estimates suggesting that up to one in five (20%) women may develop this condition. The risk of lymphedema depends on various factors, such as the type of treatment received, the extent of lymph node removal or radiation therapy, and personal factors such as age, weight, and overall health. That said, even if you’re at high risk of lymphedema, there are proactive steps you can take to minimize your chances of developing the condition. I share resources on how to prevent and treat lymphedema after breast cancer in Breast Cancer Rehab!
What triggers lymphedema flare-ups?
Various factors can contribute to lymphedema flare-ups, including physical trauma, infections, hormonal changes, temperature extremes, and not moving for long periods. Physical trauma, such as cuts, burns, insect bites, or even pushing yourself too hard during an exercise routine can disrupt lymphatic flow and lead to fluid buildup. Infections, such as cellulitis or lymphangitis, can cause inflammation and make lymphedema swelling worse. Hormonal changes, especially the ones associated with menstruation or menopause, can influence fluid retention. Sitting or standing for long periods can negatively impact lymphatic drainage. Every person is different and your lymphedema triggers are unique. It’s essential to understand what typically causes lymphedema flare-ups for you and do your best to avoid those triggers or take proactive steps to minimize their impact.
What does a lymphedema flare-up feel like?
A lymphedema flare-up may feel like a sudden increase in swelling, heaviness, or discomfort in the affected area, such as your arm, chest, or neck. You may get a sensation of tightness or fullness, as well as a feeling of warmth or tingling. If you have lymphedema in your arm, moving it may become more challenging, and there may be a noticeable change in the size or shape of your arm. You may also feel pain, achiness, or a sensation of pressure. It’s important to pay attention to the changes in your body and take proactive steps to minimize swelling (such as wearing a compression garment or doing manual lymph drainage) if you feel a lymphedema flare-up coming.
Get More Support in Breast Cancer Rehab
Life after breast cancer treatment can be confusing. It’s possible to live fully after breast cancer, but it’s not always easy to figure out how to recover and manage uncomfortable physical symptoms (along with draining emotions).
Unfortunately, there’s a lack of reputable information on life after breast cancer and how to prevent chronic conditions like lymphedema from developing. As a physical therapist and a Certified Lymphedema Specialist, I’ve seen many people who have told me that their doctor brushed off their symptoms as “the new normal.”
In Breast Cancer Rehab, I share comprehensive education, resources, and exercises that’ll help you minimize your risk of lymphedema and manage other breast cancer side effects, such as cording, scar tissue, and more.
The truth is, there are steps you can take to build up your strength and minimize your risk of lymphedema. Lymphedema after breast cancer may be common, but it doesn’t have to be normal for you.