Receiving a lymphedema diagnosis can be scary. You might find yourself searching for answers about how this condition will affect your future and wondering about lymphedema life expectancy.
With proper management and consistent treatment, most people with lymphedema can enjoy a normal life expectancy and maintain a high quality of life.
However, it’s important to understand that neglecting treatment or inconsistently following your management routine can lead to complications that may impact your quality of life and longevity.
Taking a proactive approach to lymphedema care makes a big difference in your long-term health outcomes. You can work with a lymphedema specialist and find more support in Lower Body Lymphedema Rehab.
What Is Lymphedema?
Lymphedema is a chronic condition that causes swelling in the arms, legs, or other parts of your body. This happens when your lymphatic system can’t effectively transport lymphatic fluid, so it accumulates in your tissues.
There are two main types of lymphedema:
- People with primary lymphedema are born with a lymphatic system that didn’t form correctly. In this case, symptoms may appear at birth or develop later in childhood, adolescence, or even adulthood. This type is relatively rare, affecting only 1 in 100,000 people.
- Secondary lymphedema is much more common and develops after damage to a previously normal lymphatic system. It’s often caused by surgery and cancer treatment, especially if your lymph nodes were removed, or radiation therapy that damages lymphatic vessels.
Other causes of lymphedema include trauma, infection, obesity, and certain parasitic infections in tropical regions.
Common symptoms of lymphedema include persistent swelling in an arm, leg, or affected body part, a feeling of heaviness or tightness, restricted range of motion, discomfort, recurring infections, and hardening or thickening of the skin.
Lymphedema is a chronic condition with no known cure, but it has a normal life expectancy as long as you’re following proper treatment to avoid complications.
Stages of Lymphedema
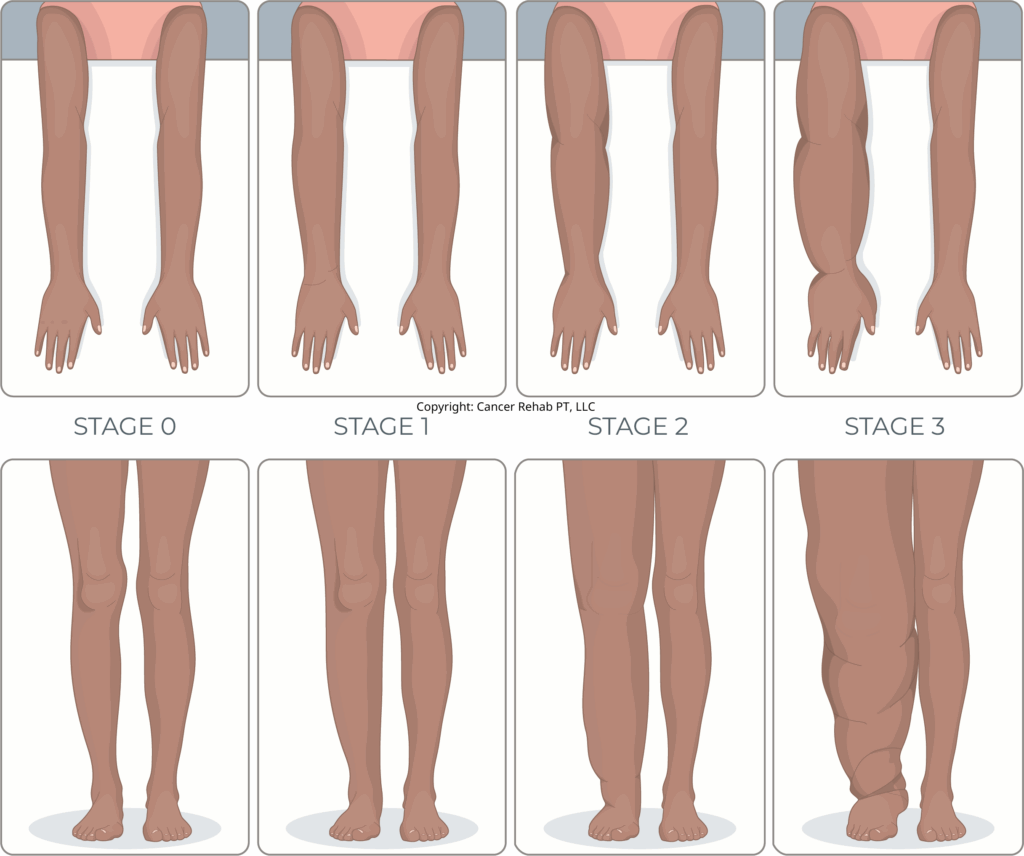
Lymphedema progresses through four distinct stages, from latent (Stage 0) to severe (Stage 3). With proper treatment and management, you can often stop lymphedema from advancing to later stages.
Stage 0 (Latent)
During this early stage, you won’t notice any visible swelling yet. However, changes are happening beneath the surface. You might experience:
- A feeling of heaviness in the affected limb
- Slight discomfort or aching
- Tingling sensations
- No obvious swelling that others can see
Many people don’t realize they have lymphedema at this stage, but beginning treatment now can prevent progression or even naturally reverse lymphedema.
Learn more about preventing lymphedema and recognizing early lymphedema signs.
Stage 1 (Early & Mild)
At this stage, visible swelling appears that typically improves when you elevate the affected limb. Your symptoms may include:
- Soft swelling that leaves a temporary dent when pressed (pitting edema)
- Feeling of fullness or heaviness in the limb
- The swelling often reduces overnight or with elevation
- Mild discomfort during activities
- Tight-feeling skin
With proper treatment, Stage 1 lymphedema can often be well-managed and sometimes even reversed with physical therapy.
Stage 2 (Moderate)
At Stage 2, lymphedema symptoms typically include:
- More persistent swelling that doesn’t improve much with elevation
- Firmer affected tissue that feels less “denty” when pressed
- Hardening and thickening of the skin (fibrosis)
- Deeper skin folds
- Increased risk of infections
- More difficulty with daily activities
Lymphedema treatment and self-care practices like wearing compression garments can help you manage symptoms, prevent complications, and improve your quality of life.
Stage 3 (Severe)
At this advanced stage of lymphedema, people typically experience:
- Permanent, hard swelling that doesn’t respond to elevation
- Severely hardened skin with a leathery texture
- Very deep skin folds
- Recurring infections become common
- Skin changes, including thickening, discoloration, and growth-like protrusions
- Significant limitation in mobility and daily activities
- Increased risk of serious complications like cellulitis and lymphangiosarcoma (a rare cancer)
Stage 3 lymphedema requires intensive management to prevent complications that can impact both quality of life and life expectancy. But even at this advanced stage, proper treatment can still provide lymphedema patients relief and prevent further complications.
However, if left untreated, severe lymphedema can become life-threatening because of complications.
What Is the Life Expectancy of a Person With Lymphedema?
For most people, lymphedema life expectancy is normal when the condition is properly managed. With appropriate lymphedema treatment and consistent self-care, you can lead a full and active life.
The key factor affecting life expectancy isn’t the lymphedema diagnosis itself, but how well you manage the condition over time. If you follow your treatment plan, you can minimize swelling and other uncomfortable symptoms, especially with early detection.
However, neglected lymphedema can lead to infections like cellulitis, which may cause long-term health issues and impact longevity.
How Fast Does Lymphedema Progress?
It depends. Some people can stay at Stage 0 or 1 for years or even decades with proper management. Without treatment, lymphedema typically progresses gradually over months to years.
How fast lymphedema progresses can be influenced by:
- Initial cause of lymphedema (primary vs. secondary)
- Extent of lymphatic system damage
- Consistency of treatment and self-care
- Presence of risk factors like obesity or recurring infections
- Individual differences in lymphatic function
Many people first notice lymphedema symptoms shortly after surgery or cancer treatment, especially when lymph nodes have been removed. For example, you may develop arm or breast swelling after a double mastectomy.
The highest risk for developing lymphedema after cancer surgery happens in the first year, and it begins to decrease after that.
However, it unfortunately never goes down to 0. Lymphedema can appear months or even years after treatment.
This delayed onset often catches people by surprise, leading them to dismiss early warning signs like occasional swelling or heaviness in a limb. If you notice any tingling or fluid retention issues after surgery or cancer treatment, try to see a certified lymphedema therapist as soon as possible.
How to Prevent Lymphedema From Progressing?
If you develop lymphedema, the best way to stop it from progressing is to get a proper diagnosis early and keep up with your treatment plan.
The sooner lymphedema is identified, the better your outcomes will likely be.
After receiving an accurate diagnosis, you’ll need to:
- Follow your treatment plan consistently: This typically includes compression therapy, exercise, skin care, and manual lymphatic drainage.
- Maintain a healthy weight: Excess weight puts additional strain on your lymphatic system and can make lymphedema symptoms worse.
- Protect the affected area: Avoid injuries, sunburn, bug bites, and tight clothing or jewelry that could restrict lymphatic flow or trigger inflammation.
- Watch for and promptly treat infections: Skin breaks, redness, warmth, or increased swelling could indicate an infection like cellulitis that requires immediate medical attention.
You should work with a certified lymphedema therapist and regularly follow up with your medical team.
You can also find more support in my programs, Lower Body Lymphedema Rehab and Breast Cancer Rehab, for more education and management practices you can do at home.
What Is the Most Effective Treatment for Lymphedema?
Lymphedema treatment follows a two-phase approach.
First comes Complete Decongestive Therapy (CDT), an intensive treatment period usually supervised by healthcare professionals. This is followed by an at-home maintenance phase that you’ll continue for life.
Complete Decongestive Therapy (CDT)
Complete Decongestive Therapy is the gold standard treatment for lymphedema. It typically includes:
- Manual Lymphatic Drainage (MLD): Special gentle massage techniques that help move lymph fluid from congested areas to functioning lymph vessels.
- Compression Therapy: The use of bandages, garments, or devices that apply pressure to help fluid move and prevent its re-accumulation.
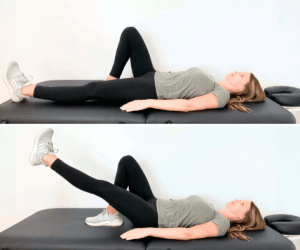
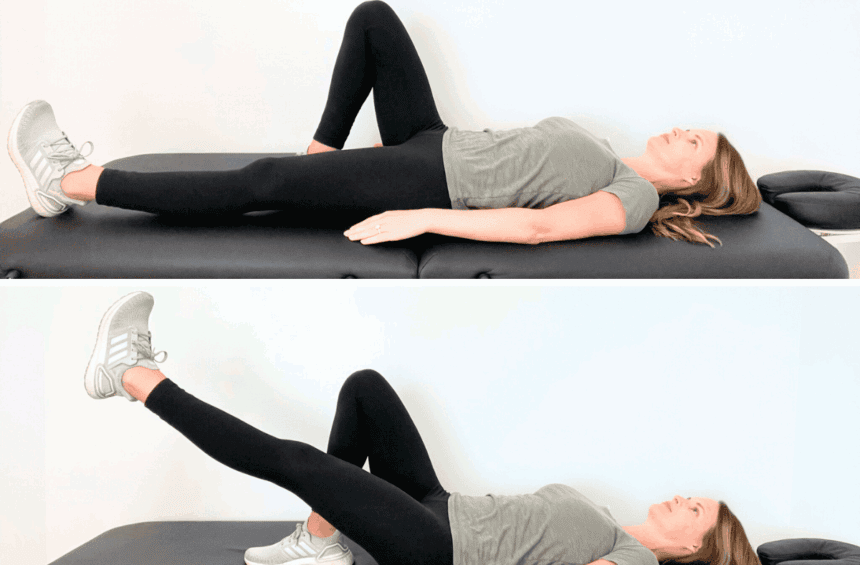
- Exercise: Specific movements to activate muscles that help pump lymph fluid through your body.
- Skin Care: Cleaning and moisturizing your skin to keep it healthy and prevent infections.
- Education: Learning the self-care techniques you’ll use during the maintenance phase.
CDT is typically provided by certified lymphedema therapists several times per week for a few weeks to a few months, depending on the severity of your condition.
Lymphedema Self-Care
After the intensive CDT phase, you’ll transition to lymphedema self-care. Since lymphedema is a lifelong disease, it’s something that you’ll continue doing at home long-term to prevent fluid buildup.
Lymphedema self-care can look different for different people because you may respond to certain treatment options better than others. That said, it usually includes:
- Self-MLD: Performing lymphatic drainage techniques on yourself to support your lymph system.
- Daily compression: Wearing properly fitted compression garments during waking hours (and sometimes during nighttime).
- Regular exercise: Following a physical therapy program or engaging in low-impact exercise such as walking and swimming to improve lymph drainage. Try these exercises for breast lymphedema.
- Meticulous skin care: Keeping your skin clean, moisturized, and protected from injury to prevent skin infections.
- Weight management: Staying at a healthy weight reduces the strain on your lymphatic system.
Unfortunately, getting access to ongoing support when living with lymphedema is often hard and expensive. Many people can’t see a certified lymphedema therapist regularly.
You can find physical therapy exercises and self-care practices to reduce swelling in Lower Body Lymphedema Rehab and Breast Cancer Rehab.
Emotional Support
Living with a chronic condition like lymphedema affects not just your physical health but your emotional well-being, too.
You can find support through lymphedema groups, counseling, or connections with others who have the condition. Many people find that sharing experiences and tips with people who understand their challenges helps them cope better.
Is Lymphedema a Disability?
Lymphedema isn’t automatically recognized as a disability, but it can qualify for disability benefits depending on its severity and impact on your life.
The Social Security Administration (SSA) doesn’t list lymphedema specifically in its “Blue Book” of disabling conditions. But you may still qualify for Social Security Disability benefits if:
- Your lymphedema symptoms match the criteria for other listed conditions, such as “Major Dysfunction of a Joint” (if lymphedema severely limits your arm or leg movement) or “Chronic Venous Insufficiency” (if swelling affects two-thirds or more of your legs).
- Your lymphedema is related to cancer treatment.
- Your symptoms prevent you from working (through what’s called a “medical vocational allowance”).
For workplace accommodations, the Americans with Disabilities Act may apply if your lymphedema limits major life activities.
Can I Live a Long Life with Lymphedema?
Yes, you can live a long and fulfilling life with lymphedema. With proper management and care, most people with lymphedema have a normal life expectancy.
As a certified lymphedema therapist, I’ve unfortunately seen many people who were told by their doctors that they should just accept swelling and limitations as their new normal. That is not true.
There are ways to effectively manage lymphedema and even naturally reverse swelling, especially in the earlier stages. Lymphedema life expectancy can be normal for many people.
Severe Lymphedema and Potential Complications
Lymphedema itself doesn’t shorten your life expectancy, but severe, untreated, or poorly managed lymphedema can lead to serious complications. These complications can sometimes be life-threatening.
- Recurrent infections: The most significant complication is cellulitis, which is a bacterial skin infection that may require hospitalization and, in rare cases, can lead to sepsis.
- Lymphangiosarcoma: This rare form of soft tissue cancer can develop in long-standing, severe cases of lymphedema, especially if it’s related to breast cancer treatment.
- Impaired mobility: Advanced lymphedema can significantly limit your movement and activity, which can trigger secondary health problems that come with a sedentary lifestyle.
- Skin changes and ulcers: Severe lymphedema can cause thickening of the skin (fibrosis), wart-like growths (papillomas), and in some cases, ulcers that are difficult to heal and prone to infection.
Fortunately, most of these serious complications can be prevented with proper lymphedema management. Early intervention is ideal, but even advanced lymphedema can improve with treatment.
FAQs
At What Stage Is Lymphedema Reversible?
Lymphedema is most reversible during Stage 0 (latent) and early Stage 1, when swelling is still mild. During these early stages, proper treatment can reduce swelling to the point where it’s barely noticeable. However, the underlying lymphatic damage typically remains. This is why many healthcare professionals use the term “managed” rather than “cured” or “reversed.”
How Bad Does Lymphedema Get?
If you don’t manage your lymphedema symptoms, the swelling can eventually progress from mild to severe. In advanced lymphedema, your limbs can become extremely enlarged and misshapen, with hardened, thickened skin that develops deep folds and sometimes growths called papillomas. It can become difficult to move and do your daily activities, such as dressing or working. However, even severe lymphedema can be improved with intensive treatment.
Can Lymphedema Put You in a Wheelchair?
Yes, but usually only in severe cases that affect your legs. This typically happens in advanced Stage 3 lymphedema, where swelling, skin changes, and repeated infections create too much heaviness and pain to move normally.
Can You Drive a Car with Lymphedema?
Yes, many people with lymphedema can safely drive a car with minimal restrictions. You may want to consider some adaptations to make driving more comfortable. For example, with arm lymphedema, you might need steering wheel adaptations or padding for comfort. With leg lymphedema, you’ll probably feel more comfortable with automatic transmission vehicles to reduce the need for constant pedal pressure. Make sure to take frequent breaks during long drives to help with the swelling.
Is Your Immune System Compromised If You Have Lymphedema?
Lymphedema doesn’t weaken your entire immune system, but it does create a weak spot in the affected limb. Your lymphatic system helps fight infections by moving immune cells and antibodies throughout your body. When lymphedema blocks this flow in an arm or leg, those infection-fighting cells can’t reach that area easily. This is why even small cuts or scrapes on a lymphedema-affected limb can more easily develop into serious infections like cellulitis. The rest of your body maintains normal immune function, but that specific area is more vulnerable.
Minimize Lymphedema Symptoms with Lower Body Lymphedema Rehab
Lymphedema life expectancy is normal, and many people enjoy active and fulfilling lives with minimal restrictions, especially after early detection.
Proper management can help you keep the swelling under control and prevent serious complications. Lymphedema only becomes life-threatening when left untreated.
If you’ve received a lymphedema diagnosis or want to minimize your chances of getting lymphedema after cancer treatment, you can find support in Lower Body Lymphedema Rehab and Breast Cancer Rehab.