Lymphedema causes swelling in your legs because of lymph fluid build-up, and it can be very uncomfortable and limiting. While there’s no cure for lymphedema, there are effective ways to treat leg lymphedema to reduce swelling, prevent complications, and improve your quality of life.
As a certified lymphedema therapist (CLT-LANA) and physical therapist, I’ll walk you through 7 proven methods that encourage lymph fluid drainage and help you live a more comfortable life.
What Is Leg Lymphedema?
Lymphedema is a chronic medical condition with no known cure, but it is treatable.
When lymphatic fluid backs up in your legs, it causes swelling that can range from mild to severe. This happens because your lymphatic system, the network responsible for draining extra fluid from your tissues, isn’t working properly.
There are two types of lymphedema: primary and secondary.
Primary lymphedema is typically genetic. Some people are born with it, and others develop it during childhood or early adulthood. Primary lymphedema is rare, affecting about 1 in 100,000 people.
Secondary lymphedema develops after something damages or disrupts your lymphatic system. Cancer treatment is the most common cause, especially when lymph nodes are removed or damaged during surgery or radiation therapy.
Other causes include trauma, infection, or injury to the lymphatic system. Secondary lymphedema affects approximately 1 in 1,000 Americans, so it’s far more common than the primary form.
How Serious Is Lymphedema in the Legs?
If you develop lymphedema, it’s important to treat it seriously. It doesn’t reduce your life expectancy, but without treatment, the condition will progress and get worse over time.
As swelling increases, your legs become heavier and more difficult to move.
Your risk of infection also goes up a lot, and a condition called cellulitis can develop when bacteria enter through compromised skin. This infection can be very dangerous, and it’ll require antibiotics.
Many of my patients come to me after years of living with uncomfortable lymphedema symptoms because they didn’t have access to proper treatment resources. They struggle with pain, limited mobility, and frequent infections, but this isn’t inevitable.
With the right treatment approach, you can reduce swelling, prevent complications, and maintain or improve your quality of life.
Learn more about when lymphedema can turn dangerous.
How to Treat Leg Lymphedema
The gold standard treatment for lymphedema is called Complete Decongestive Therapy (CDT). It happens in two phases:
Phase 1 is the intensive treatment phase, where you work with a certified lymphedema therapist several times a week. During this phase, your therapist uses manual lymphatic drainage, compression bandaging, exercises, and skin care to reduce your swelling as much as possible.
Phase 2 is the maintenance phase, where you continue many of the same activities at home as lymphedema self-care to maintain your progress.
Along with CDT, other tools and techniques can help you reduce and manage swelling. Let me walk you through the most effective options:
1. Elevation
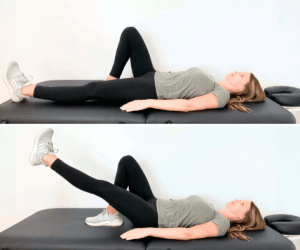
A simple way to reduce swelling is with elevation, especially for early-stage lymphedema.
Gravity is not leg swelling’s best friend. Your lymphatic vessels and veins have to pump up against gravity during the day, which can be difficult when your lymphatic system is already struggling.
Elevating the legs above your heart for 30 minutes can help the fluid move out of the legs.
However, if you have moderate or severe swelling, this approach may not be very effective in opening up your fluid flow. Luckily, there are other ways to reduce lymphedema swelling!
2. Compression Garments
Compression therapy is one of the most important and effective ways to manage leg lymphedema. Compression stockings (also called compression garments) are designed to support your lymphatic system and prevent fluid from accumulating in your legs.
Before you start wearing compression stockings, the gold-standard approach is to go through 2-5 weeks of compression bandaging with a certified lymphedema therapist.
These bandages are called short-stretch bandages, and they work differently from regular ACE bandages. Your therapist wraps your legs using these special bandages along with cotton padding and foam padding to reduce the volume and size of your leg as much as possible.
I recommend these bandages:
Once your leg is as small as we can get it, you transition into a compression stocking or garment.
There are a few different options:
- Circular knit garments are elastic and usually come ready-to-wear in standard sizes. The typical medical-grade compression level is 20-30mmHg, though other levels are available. These garments work well for mild swelling.
- Flat knit garments are inelastic and usually custom-made, though a few options like the Solaris ExoStrong come pre-sized. These garments are best for moderate to severe lymphedema because they do a better job of preventing swelling from building up.
- Velcro wraps are another excellent option if you have difficulty getting compression stockings on and off. This favorite of mine offers good compression and makes lymphedema management more accessible for many people.
Learn how to put on compression socks.
3. Manual Lymph Drainage
Lymphatic drainage (also called lymphatic drainage massage) is a specialized, gentle technique that helps move lymphatic fluid through your lymph vessels and out of the swollen area.
This massage uses very light pressure with the whole hand, following a specific sequence and direction to guide fluid to your working lymph nodes.
A certified lymphedema therapist will teach you how to do this technique on yourself during CDT. Once your doctor clears you, you can do lymphatic drainage at home as part of your daily self-care routine.
You can also follow one of my lymphatic drainage massage guides:
Modified Lymphatic Drainage Diagram for Moderate to Severe Lymphedema in the Left Leg – Digital
Modified Lymphatic Drainage Diagram for Moderate to Severe Lymphedema in the Right Leg – Digital
4. Physical Exercise
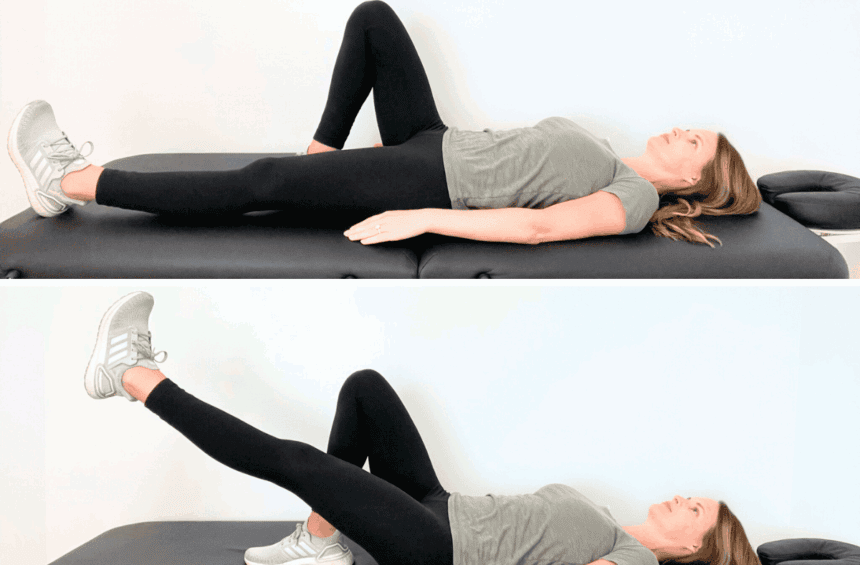
Exercise and movement are essential for lymphedema management. Your muscles act as a pump for both your lymphatic system and your veins. When you contract and stretch your muscles, you stimulate these systems and help fluid move out of your legs.
If you spend most of your day sitting or lying down, try these simple exercises:
- Ankle pumps: Flex and point your feet up and down 10-20 times
- Knee bends: While sitting, straighten and bend your knees back and forth 10-20 times
- Marching: Sitting or standing, lift your knees high in an alternating marching motion 10-20 times
If you’re looking for more exercise options, swimming is great for your lymph system. The water adds natural compression to your body, similar to what a compression stocking does.
Rebounding on a mini trampoline like this is another great way to stimulate trapped fluid. Vibration plate exercises can also be helpful—the gentle vibrations encourage lymphatic drainage as you stand or do simple exercises on the platform.
Learn more about vibration plates vs. rebounders and which exercise will work best for you!
5. Skin Care
Lymphedema puts you at higher risk for skin infections. The extra fluid in your tissue creates an environment where bacteria can grow more easily.
When you have swelling in your arm or leg for months or years, your skin can break down and create wounds, increasing your infection risk.
To lower your chances of infection, keep your skin and nails healthy, clean, and protected. Apply moisturizer daily to keep your skin hydrated, and always use sunscreen to avoid sunburns and insect repellent to minimize bug bites.
If you do get a cut, clean it and apply antibiotic cream right away.
6. Deep Breathing
Deep breathing or belly breathing helps stimulate your lymphatic system and move lymphatic fluid throughout your body. Your abdomen has many lymph nodes, and deep breathing creates gentle pressure that activates these nodes.
Try placing your hand on your stomach, putting light pressure inwards.
Holding this pressure, take a slow, deep breath and feel your belly expand into your hand, but keep the gentle resistance. Then slowly exhale while continuing to press lightly on your abdomen. Repeat this 3 to 5 times.
7. Weight Management
Research shows a clear connection between body mass index (BMI) and lymphedema.
Studies explain that people with a BMI over 25 are at a higher risk of developing secondary lymphedema after surgery that removes lymph nodes.
When someone’s BMI is over 40, they can develop obesity-induced lymphedema, which may stay even if you lose weight because of the permanent damage to the lymphatic system.
If you already have lymphedema and carry extra weight, losing even 5 to 10 pounds can make a huge difference in how much swelling you have.
You can do this through a healthy diet and exercise.
Some of my patients have asked about GLP-1 medications for lymphedema.
Medications like Ozempic or Wegovy can lead to weight loss and help reduce swelling, but they don’t repair lymphatic damage.
They can be a helpful tool as part of your overall treatment plan, but they’re not a cure and don’t replace compression therapy, lymphatic drainage, exercise, and other physical therapy treatments.
What Happens If Lymphedema Is Left Untreated?
Without treatment, lymphedema gets worse over time.
You’ll experience more swelling, which will make your legs heavier and harder to move. Your risk of infections like cellulitis will also go up, which can be dangerous and require hospitalization.
Overall, the longer lymphedema goes untreated, the harder it becomes to manage.
If you’ve had radiation therapy, cancer surgery, or another procedure that had to do with your lymph nodes, make sure to watch out for lymphedema symptoms to get medical treatment as soon as possible.
Don’t know where to start? Try this FREE lymphedema self-care guide:
Does Leg Lymphedema Ever Go Away?
No, unfortunately, leg lymphedema doesn’t go away on its own. It’s a chronic condition, but it doesn’t mean that you have to accept constant swelling and discomfort as a normal part of your life.
You can manage lymphedema to reduce swelling, and many of the patients I see in the physical therapy clinic go on to have normal and active lives.
If you catch lymphedema in its early stages and treat it aggressively, you may be able to reverse the visible swelling, though the underlying damage to your lymphatic system will stay.
FAQs
How to cure lymphedema in the legs?
There is no cure for leg lymphedema or any other type of lymphedema. But consistent management through compression therapy, lymphatic drainage, exercise, skin care, and other treatments will help you get swelling under control and, in many cases, live a full life with minimal restrictions.
Lymphedema surgery is available to some people, but it’s still not a cure. It’s another treatment option that may help reduce swelling, but you’ll still need to continue your management routine afterward.
Is walking good for leg lymphedema?
Yes, walking is great for leg lymphedema. Like other low-impact exercises, walking contracts and stretches your leg muscles, which helps pump lymphatic fluid out of your legs. You can also try biking, swimming, yoga, vibration plates, or rebounder exercises.
What is the gold standard treatment for lymphedema?
Complete Decongestive Therapy (CDT) is the gold standard treatment for lymphedema. It combines manual lymphatic drainage, compression bandaging, exercise, and skin care in an intensive treatment phase with a certified lymphedema therapist. After reducing your swelling, you’ll do lymphedema self-care at home to maintain your results.
What should you not do with lymphedema in your legs?
Flare-up triggers vary from person to person, but common ones include wearing tight clothing (especially around your waist, thighs, or calves) and sitting or standing for long periods without movement. Ignoring lymphedema instead of actively managing it will also make the swelling worse.
Other than that, pay attention to how your legs respond to different activities, foods, or situations. Some people notice that their swelling becomes worse with certain foods, hot weather, air travel, or other activities. Track what triggers your flare-ups so you can avoid or prepare for them.
What type of doctor treats lymphedema of the legs?
To treat lymphedema, you’ll usually work with a certified lymphedema therapist (CLT), who is often a physical therapist, occupational therapist, or massage therapist with specialized training. Your primary care doctor or oncologist can refer you to a CLT.
Learn more about the doctors who treat lymphedema.
Can compression garments make lymphedema worse?
Yes, if they’re not fitted properly. Compression garments that are too tight can create a tourniquet effect, blocking fluid flow and making the swelling above or below the garment worse. In turn, garments that are too loose won’t provide enough compression to be effective.
To avoid these issues, work with a certified fitter who can take your measurements and make sure that the garment fits correctly.
Get More Support with Your Lymphedema Treatment
Managing leg lymphedema on your own can feel overwhelming, especially when access to certified lymphedema therapists is limited or expensive.
That’s why I created the Lower Body Lymphedema Rehab program—an affordable and comprehensive resource that teaches you how to effectively manage your symptoms at home.
You’ll get the same knowledge and techniques I teach my patients in the clinic, but at a fraction of the cost of in-person physical therapy. You’ll get:
- Education on lymphedema stages, treatment, and Complete Decongestive Therapy
- Manual lymphatic drainage techniques you can do yourself at home
- Bandaging routines to reduce swelling
- Compression therapy guidance, including how to choose and use day garments and nighttime garments
- Physical therapy exercises to manage leg swelling
- Skin care recommendations to lower your risk of infection
- Deep breathing exercises to stimulate lymphatic flow
- Kinesiology taping tips for more support for your swollen limb
- Information on medical solutions like pneumatic compression pumps and surgical options
- Healthy lifestyle habits that support lymphedema management
Even small changes in your lymphedema management routine can lead to big results.
Learn more about Lower Body Lymphedema Rehab and join today!