If you’ve been diagnosed with lymphedema, you’re probably wondering who can help you manage this condition. Your most important resource will be a certified lymphedema therapist (CLT), a healthcare professional with specialized training in lymphedema management.
Lymphedema causes swelling in your arms, legs, or other areas of your body due to a buildup of lymph fluid. It’s a chronic condition, but it can be effectively managed. Many people lead active and fulfilling lives with lymphedema, only experiencing minimal restrictions.
I’m Kelly Sturm, a Doctor of Physical Therapy (PT, DPT) and Certified Lymphedema Therapist (CLT-LANA). I’ve created several resources to help you improve lymphedema symptoms, including Lower Body Lymphedema Rehab, Breast Cancer Rehab, and Digital Guides.
What Is Lymphedema?
Lymphedema is chronic swelling. It happens when your lymphatic system can’t properly drain lymph fluid from your tissues, most often in your arms or legs, though it can affect other body parts too.
There are two main types of lymphedema:
- Primary lymphedema is rare and present from birth, caused by problems with lymphatic system development.
- Secondary lymphedema is much more common, affecting up to 250 million people worldwide. It develops after damage to your lymphatic system, often after cancer treatments like lymph node removal or radiation therapy.
Common symptoms of lymphedema include swelling, heaviness, tightness, limited movement, hardening of the skin, and recurring infections. Lymphedema doesn’t have a cure, but proper treatment can significantly reduce swelling and improve your quality of life.
Who Is the Best Doctor to See for Lymphedema?
In most cases, you should be seeing a certified lymphedema therapist (CLT). However, you might work with a few different healthcare providers depending on your specific situation.
Your lymphedema treatment team could include physical therapists, occupational therapists, your oncologist, a nutritionist, or sometimes a surgeon.
Certified Lymphedema Therapist (CLT)
A certified lymphedema therapist has special training in lymphedema treatment. They can be physical therapists, occupational therapists, massage therapists, or other medical professionals, but they all complete a rigorous 135-hour course to earn their certification.
Your CLT will create a personal treatment plan for you and show you how to handle lymphedema at home. They’re skilled in special techniques like lymphatic drainage massage and will teach you how to take care of your skin, use compression garments, and do special exercises to manage swelling.

Physical Therapist
Physical therapists help improve your movement and strength. For lymphedema, they focus on exercises that encourage lymph fluid drainage. They might work on your range of motion, strength, and balance to help you stay active with lymphedema.
Many physical therapists get additional certification to become CLTs and specialize in physical therapy for lymphedema.
Occupational Therapist
Occupational therapists help you do everyday activities more easily. With lymphedema, they teach you ways to protect your affected limb while doing daily tasks. They might suggest special tools or new ways to do things that put less strain on your swollen arm or leg.
Like physical therapists, many occupational therapists also get certified as CLTs.
Oncologist
If your lymphedema developed as a result of cancer treatment, your oncologist will likely stay involved in your care. They’ll monitor both your cancer recovery and how lymphedema affects you. They can also refer you to lymphedema specialists.
Unfortunately, lymphedema is a common side effect after cancer treatment, especially after breast cancer. It’s estimated that 1 in 5 women treated for breast cancer have breast cancer-related lymphedema.
However, early diagnosis and treatment can make a big difference in how much lymphedema swelling you have.
Nutritionist
Weight management can help improve or even prevent lymphedema. A nutritionist can help you maintain a healthy weight and suggest foods that might reduce inflammation and swelling.
Surgeon
In some cases, a surgeon specializing in lymphatic procedures might be part of your team. They perform specialized surgeries like lymph node transplant or lymphovenous bypass to improve lymphatic fluid drainage.
These surgical treatments don’t cure lymphedema but may reduce symptoms in some people.
What Is the Most Common Treatment for Lymphedema?
The standard approach to treating lymphedema happens in two main phases: Complete Decongestive Therapy (CDT) and ongoing self-care. First, you’ll work with a lymphedema therapist for intensive treatment to reduce swelling. Then, you’ll learn how to manage your condition daily at home.
This will help control the swelling and prevent it from getting worse over time.
Complete Decongestive Therapy
Complete Decongestive Therapy (CDT) is the first phase of lymphedema treatment. You’ll visit a lymphedema therapist regularly for several weeks for hands-on care.
During these sessions, your therapist will:
- Give you manual lymphatic drainage (MLD), a gentle massage technique that helps move fluid out of swollen areas
- Wrap your affected limb with special bandages to reduce swelling
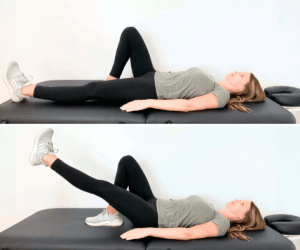
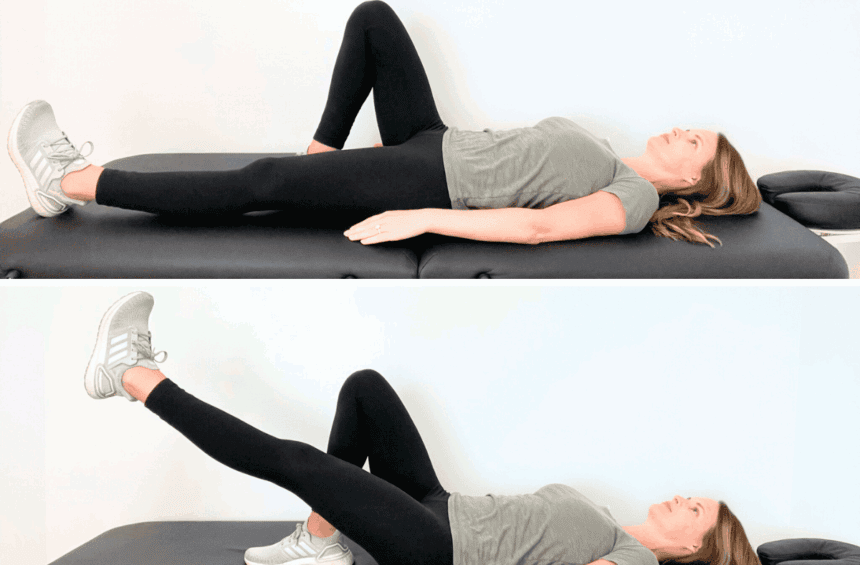
- Teach you specific exercises that help lymph fluid move through your body
- Show you how to take care of your skin to prevent infections
Most lymphedema patients see significant improvement during this phase, with reduced swelling and better mobility. The goal is to get the swelling down as much as possible before moving to the self-care phase.

Lymphedema Management
After the initial treatment phase, you’ll need to continue lymphedema self-care at home. This typically includes:
- Wearing your compression garments as recommended
- Doing your lymphedema exercises
- Practicing manual lymph drainage massage techniques
- Keeping your skin clean and moisturized to prevent cracks and infection
- Staying active with lymphedema-friendly activities like walking, swimming, or yoga
- Maintaining a healthy weight
- Avoiding extreme heat and protecting your affected limb from injuries
- Elevating the swollen area when resting or sleeping
It’s important to experiment with different lymphedema therapy approaches and create a routine that works for you. You don’t need to spend hours on lymphedema care every day. Consistent, small efforts make a big difference in controlling swelling and preventing complications.
Lower Body Lymphedema Rehab and Breast Cancer Rehab have many practical resources on managing lymphedema.
How Do I Find a Lymphedema Specialist?
You should look for a lymphedema specialist with proper training and experience. The most qualified specialists have certification from the Lymphology Association of North America (LANA).
LANA is a respected organization that sets high standards for lymphedema care. Their certified therapists have completed extensive training and passed rigorous exams.
To find a LANA-certified specialist near you, you can use their certified specialist search tool.
You can also ask your primary doctor or oncologist for recommendations. Some hospitals and cancer centers have lymphedema programs with certified therapists.
When choosing a specialist, consider whether they accept your insurance and how close they are to your home, as you’ll likely need multiple visits.
Preparing for Your Appointment
Going to your first lymphedema appointment prepared helps you get the most from your visit. Consider asking your lymphedema specialist the following questions:
- What type of lymphedema do I have?
- How many treatment sessions will I need?
- What will a typical session include?
- What compression garments do you recommend?
- How can I prevent flare-ups?
- What exercises are safe for me?
- What activities should I avoid?
- When should I call you if problems develop?
In turn, your lymphedema specialist will also have a few questions for you. They might ask:
- When did you first notice swelling?
- What makes your swelling better or worse?
- Have you had any skin infections in the affected area?
- Have you had cancer surgery or treatment?
- What activities or work do you do daily?
- What medications are you taking?
- Do you have any other health conditions?
- Have you tried any lymphedema treatments before?
They might also do an MRI, a CT scan, or an ultrasound to confirm your lymphedema diagnosis and rule out other potential causes of swelling, such as cancer recurrence or a blood clot (deep vein thrombosis).
Bring a list of all medications you take and notes about when your swelling started or changed. Wear loose, comfortable clothing that makes it easy to examine the swollen limb or area.
Consider bringing someone with you to help remember information, especially at your first appointment when you’ll receive a lot of new instructions.
Ongoing Lymphedema Management
Lymphedema is a chronic condition, so you’ll need to create a supportive routine to manage it long-term. Early-stage lymphedema is often responsive to treatment methods, but advanced lymphedema can cause dangerous infections like cellulitis when not treated consistently.
However, regular physical therapy for lymphedema isn’t always accessible. Many people struggle to get consistent care due to cost barriers, insurance limitations, or living far from qualified specialists.
I understand these challenges, which is why I’ve created resources you can use at home. As a certified lymphedema therapist (CLT-LANA), I’ve developed programs and digital guides for ongoing lymphedema management.
- Lower Body Lymphedema Rehab: A practical, in-depth program on managing lymphedema of the lower body, including leg, ankles, and feet.
- Breast Cancer Rehab: A physical therapy program after breast cancer treatment to prevent or minimize your risk of developing lymphedema after breast cancer surgery or radiation therapy.
- Digital Guides: An extensive library of physical therapy exercises and manual lymphatic drainage techniques to manage symptoms of lymphedema.
These resources don’t replace personalized medical care, but they give you practical tools to maintain progress and prevent complications. Having accessible resources can increase your confidence in managing lymphedema day-to-day.
FAQs
Do vascular doctors treat lymphedema?
Vascular doctors (vascular surgeons) sometimes treat lymphedema, but they’re not typically the first specialists to see. Vascular doctors specialize in blood vessels, and lymphedema involves the lymph system and lymphatic vessels. Some vascular surgeons have additional training in lymphatic disorders and may offer specialized surgical procedures for severe lymphedema.
However, most lymphedema care starts with a certified lymphedema therapist rather than a vascular doctor. If surgical options become necessary, your CLT might refer you to a vascular surgeon with lymphedema expertise.
Does insurance cover lymphedema surgery?
It depends. Some insurance companies cover lymphedema surgeries when deemed medically necessary and after conservative treatments have failed. Pneumatic compression and compression garments are often covered, but surgical treatments (for example, a vascularized lymph node transfer) are more tricky. The best thing to do is to get in touch with your insurance company.
What is the life expectancy of a person with lymphedema?
Lymphedema itself doesn’t reduce life expectancy when properly managed. Most people with lymphedema live normal lifespans, especially with good self-care practices and treatment. The main concerns are preventing and promptly treating infections like cellulitis, which can quickly become serious. Risk factors typically only rise in untreated or poorly managed cases of lymphedema.
What happens if lymphedema goes untreated?
Untreated lymphedema continues to get worse over time. Initially, swelling might come and go, but eventually, it becomes permanent and more severe. The affected limb can develop fibrosis (hardening of tissues) and thickened skin. Untreated lymphedema also significantly increases your risk of recurring skin infections (such as cellulitis) that can require hospitalization. Eventually, daily activities like walking or cooking can become difficult as the excess fluid in your body increases.
Does lymphedema ever go away?
No, lymphedema is a chronic condition and doesn’t go away once it develops. However, with proper treatment, your symptoms can improve, and the swelling can become nearly unnoticeable. In very early stages, aggressive treatment might naturally reverse the swelling, but the underlying lymphatic system damage will remain. Treatment options like wearing compression garments and doing therapeutic exercises can help you maintain a good quality of life.
Living with Lymphedema
Lymphedema occurs when damaged lymph vessels can’t properly drain lymph fluid, causing swelling and discomfort. Living with lymphedema means making some adjustments, but you don’t have to accept swelling and discomfort as your new normal.
Many people benefit from seeing a certified lymphedema therapist (CLT). They can teach you how to wear compression garments, do physical therapy exercises, and take care of your skin. However, regular access to a lymphedema therapist isn’t always possible due to location, cost, or time constraints.
If you’re looking for reliable guidance from a certified lymphedema therapist that you can access anytime, learn more about Lower Body Lymphedema Rehab and Breast Cancer Rehab.
These resources can serve as your primary support if you can’t see a therapist regularly, or they can complement your in-person therapy sessions.