When dealing with chronic swelling from lymphedema, surgery isn’t usually the first treatment option your doctor will recommend.
However, as a physical therapist & certified lymphedema therapist who’s worked with hundreds of lymphedema patients over the past decade, lymphedema surgery can play an important role in managing this condition, especially when conservative treatments aren’t providing enough relief or when the swelling has progressed to more advanced stages.
What Is Lymphedema?
Lymphedema is a chronic condition that causes swelling when your lymphatic system can’t properly drain fluid from your tissues.
This swelling typically affects your arms, legs, or other parts of your body and occurs when lymph nodes are damaged or removed, often due to cancer treatment, infection, or injury.
Lymphedema doesn’t have a known cure, but it can be effectively managed through various treatment approaches. Surgical procedures are just one option in the spectrum of care, and they’re usually only used for people who haven’t achieved adequate results with other treatments.
Researchers estimate that 1 in 30 people live with lymphedema worldwide. In the US, more people live with lymphedema than with HIV, Parkinson’s disease, multiple sclerosis, muscular dystrophy, and ALS combined.
Secondary lymphedema (swelling that occurs as a result of cancer treatment, lymph node removal, or other injury) is much more common than primary lymphedema (inherent lymphatic dysfunction).
What Are the Stages of Lymphedema?
Lymphedema progresses through four distinct stages:
- Stage 0: Your lymphatic system has been damaged, but you don’t see visible swelling yet.
- Stage 1: Swelling becomes visible but comes and goes.
- Stage 2: Swelling becomes persistent and doesn’t go away with rest or elevation.
- Stage 3: Severe lymphedema with significant, permanent swelling that changes the shape and size of your limb.
Surgery is typically considered for people with Stage 2 or Stage 3 lymphedema who haven’t responded adequately to conservative treatment, though some preventive surgical procedures might be recommended earlier in certain high-risk situations.
Lymphedema Treatment
Before considering surgery, most people with lymphedema start with conservative treatments that form the foundation of lymphedema care.
As a certified lymphedema therapist (CLT-LANA), I always start my patients with Complete Decongestive Therapy (CDT). It’s the gold standard approach. CDT combines a few different techniques to help drain the excess lymph fluid:
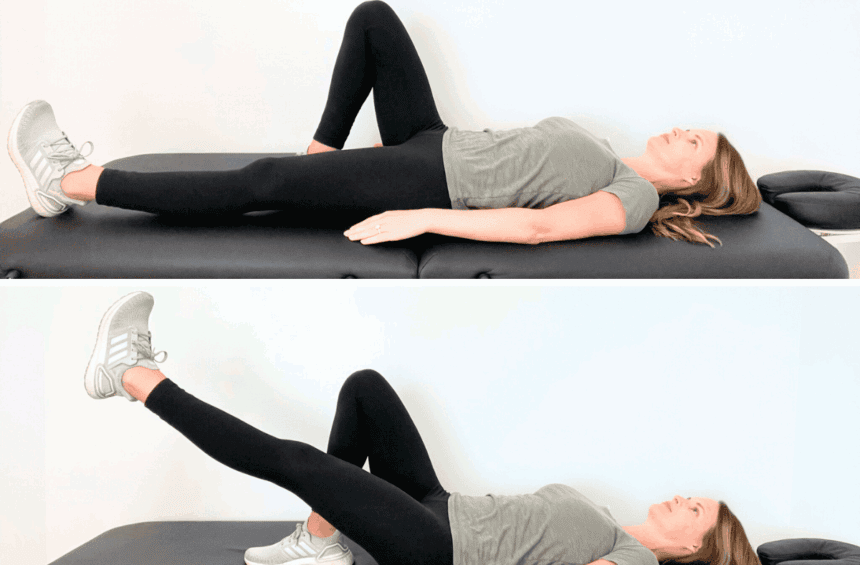
- Manual lymphatic drainage
- Compression therapy
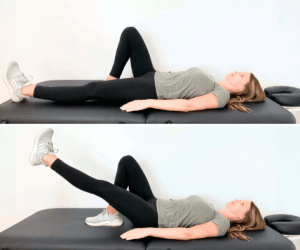
- Physical exercises
- Skin care
CDT is typically done by a certified lymphedema therapist or a physical therapist who specializes in this condition. During the initial treatment phase, you’ll work closely with your therapist to reduce swelling and learn proper techniques.
Once your swelling is under control, you’ll transition to a maintenance phase where you do lymphedema self-care at home to preserve your results.
In my experience, conservative management is enough for long-term control of swelling for most people. However, when these approaches don’t provide adequate relief or when swelling continues to progress despite consistent care, surgical treatment options may be considered.
Is There Surgery for Lymphedema?
Lymphedema surgery isn’t the primary treatment option, but there are a few procedures that can help manage the condition.
These surgeries fall into two main categories: reconstructive procedures that aim to restore lymphatic function, and ablative procedures that remove excess tissue.

Lymphaticovenous Anastomosis (Lymphovenous Bypass)
Lymphaticovenous anastomosis, also called lymphovenous bypass, is a microsurgical procedure that creates new pathways for lymphatic fluid to drain. The surgeon connects small lymphatic vessels directly to nearby veins, essentially creating a detour around the damaged lymphatic system.
This procedure works best in earlier stages of lymphedema when lymphatic vessels are still functioning, which is something I always discuss with patients who are considering this option.
Vascularized Lymph Node Transfer Surgery
This lymphatic surgery involves taking healthy lymph nodes from one part of your body and transplanting them to the area affected by lymphedema. The surgeon moves these lymph nodes along with their blood supply to help restore the lymphatic channels. Common donor sites include lymph nodes from the groin, abdomen, or neck area.
Ablative Procedures
Ablative procedures focus on removing excess tissue rather than restoring lymphatic function. These surgeries are typically considered for people with advanced lymphedema where reconstructive options may not be effective. I usually see these recommended for my patients with Stage 3 lymphedema.
Liposuction
Liposuction for lymphedema removes excess fat that has accumulated due to chronic swelling. This specialized procedure is different from cosmetic liposuction and works best for people who have been consistent with compression therapy.
After liposuction, you’ll need to wear compression garments indefinitely to maintain the results and prevent swelling from returning. This is something critical that I often see missed and often tell my patients to consider.
Charles Procedure
The Charles procedure is the most extensive lymphedema surgery, and it’s usually reserved for severe cases where other treatments haven’t worked. This procedure involves removing all skin and tissue down to the muscle, then covering the area with skin grafts. I’ve only seen this recommended one time as a last resort due to significant risks and a lengthy recovery.
Who Is a Candidate for Lymphedema Surgery?
Not everyone with lymphedema is a good candidate for surgery, and honestly, that’s often a good thing.
Generally, you may be considered for surgical treatment if you have Stage 2 or Stage 3 lymphedema that hasn’t improved enough with conservative treatments like compression therapy and manual lymphatic drainage.
You’ll also need to be healthy enough to undergo surgery.
As someone who works closely with surgical teams, I always recommend getting multiple opinions and ensuring you’ve tried all conservative options first.
What Is the Lymphedema Surgery Cost?
Lymphedema surgery can be expensive.
A 2021 study estimated costs between $22,000 and $32,000, and since then, medical costs have likely increased further. The final cost depends on factors like the complexity of the surgery, hospital fees, anesthesia, and your geographic location.
Some insurance plans cover certain procedures, especially when conservative treatments haven’t worked, but others may consider some surgeries experimental.
I always tell my patients that it’s important to check with their insurance provider about coverage and get pre-authorization when possible.
How Risky Is Lymphedema Surgery?
Like any surgery, lymphedema procedures carry risks, though the level of risk varies depending on the type of surgery. Common risks include infection, bleeding, and complications from anesthesia.
In some cases, there’s also a risk of lymphedema getting worse if the surgery is unsuccessful, which is something I’ve unfortunately seen happen more than once.
Microsurgical procedures like lymphovenous bypass and lymph node transfer have relatively low complication rates when performed by experienced surgeons. More extensive procedures like the Charles procedure carry higher risks due to their complexity.
Can You Permanently Get Rid of Lymphedema?
I wish I could tell you yes, but unfortunately, there’s no cure for lymphedema, and even surgery doesn’t completely eliminate the condition.
However, surgical procedures can significantly reduce swelling and improve your quality of life. Even after successful surgery, you’ll likely need to continue some form of lymphedema management, such as wearing compression garments and staying physically active.
FAQs
What is the surgery for lymphedema in the legs?
Surgery for leg lymphedema includes the same procedures used for arm lymphedema, such as lymphovenous bypass, lymph node transfer, liposuction, or ablative procedures. Leg lymphedema surgery can be more complex due to the size of the affected area.
Is lymphedema surgery covered by insurance?
It depends on the procedure and your insurance plan. Some insurers cover reconstructive surgeries like lymphovenous bypass or lymph node transfer, especially when you can demonstrate that conservative treatments haven’t provided adequate relief. However, coverage often requires pre-authorization, documentation of failed conservative treatment, and may be limited to certain procedures or surgeons.
Does Medicare cover lymphedema surgery?
Medicare typically doesn’t cover lymphedema surgery. However, Medicare does provide coverage for conservative lymphedema treatments, including compression garments and manual lymphatic drainage when prescribed by a doctor and deemed medically necessary.
What is the life expectancy for someone with lymphedema?
Lymphedema doesn’t affect your life expectancy when properly managed. The condition is chronic but not life-threatening, and most people with lymphedema live normal lives. However, untreated lymphedema can lead to serious complications like recurring infections (cellulitis). Consistent management with physical therapy can help you reduce swelling and live a normal life with minimal limitations.
Does lymphedema come back after surgery?
Surgery isn’t a definitive cure for lymphedema. Unfortunately, the swelling can return, especially if you don’t maintain proper lymphedema care. Surgery helps improve lymphatic drainage, but it doesn’t cure the underlying problem or restore your lymphatic system to normal function. Most people need to continue wearing compression garments and following other management strategies even after successful surgery to maintain the results.
The Bottom Line
While surgery can’t cure lymphedema and isn’t the primary form of treatment, it can be a valuable option for people whose swelling hasn’t responded adequately to conservative treatments.
However, even after a successful surgery, living with lymphedema requires ongoing care. If you were told that swelling is just something you have to live with, that’s not true. There are steps you can take to improve your symptoms, and you should exhaust all of them before considering surgery.
I share education & physical therapy exercises in my programs, Lower Body Lymphedema Rehab and Breast Cancer Rehab, and you can also find lots of lymphedema resources in my Shop.