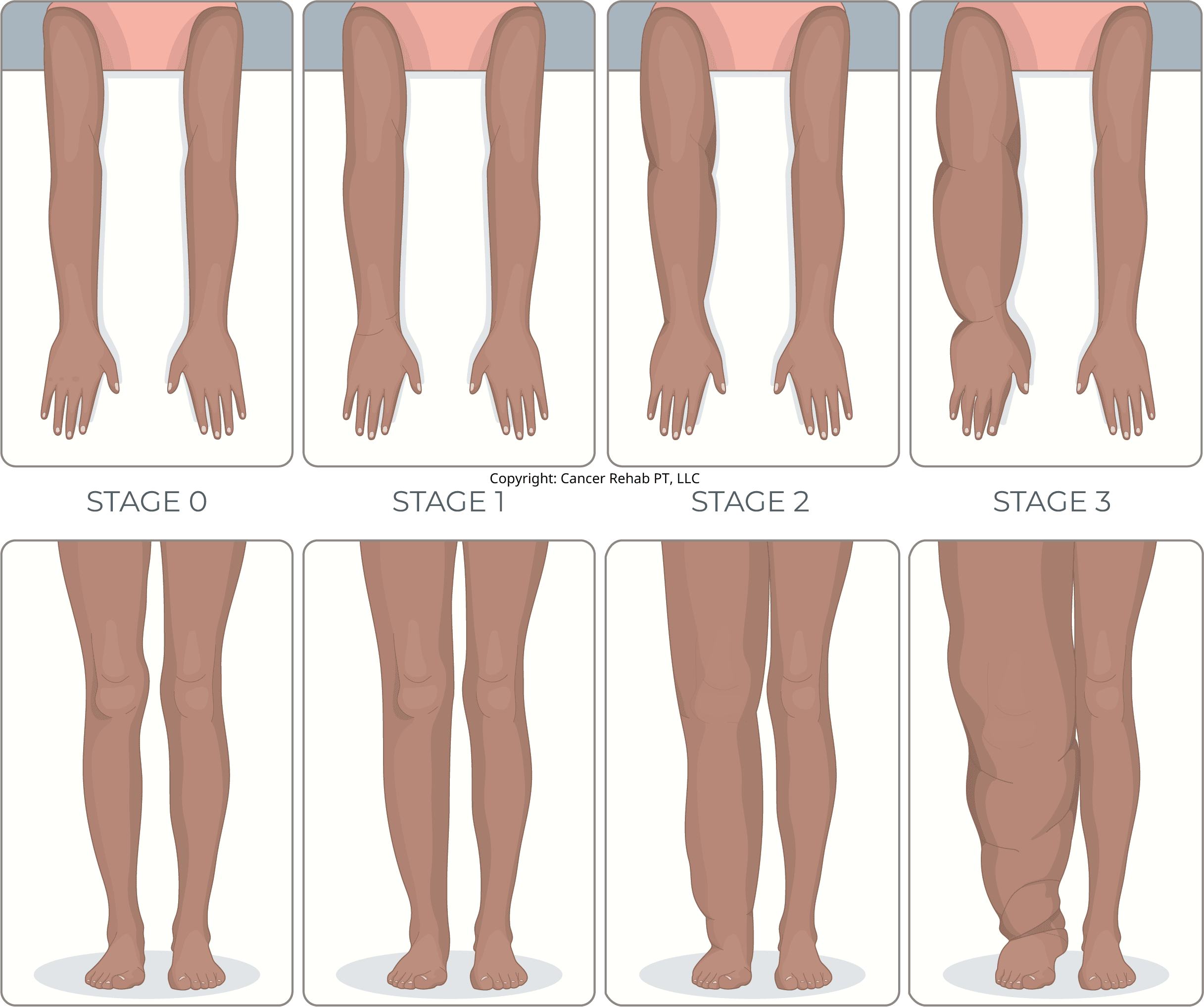
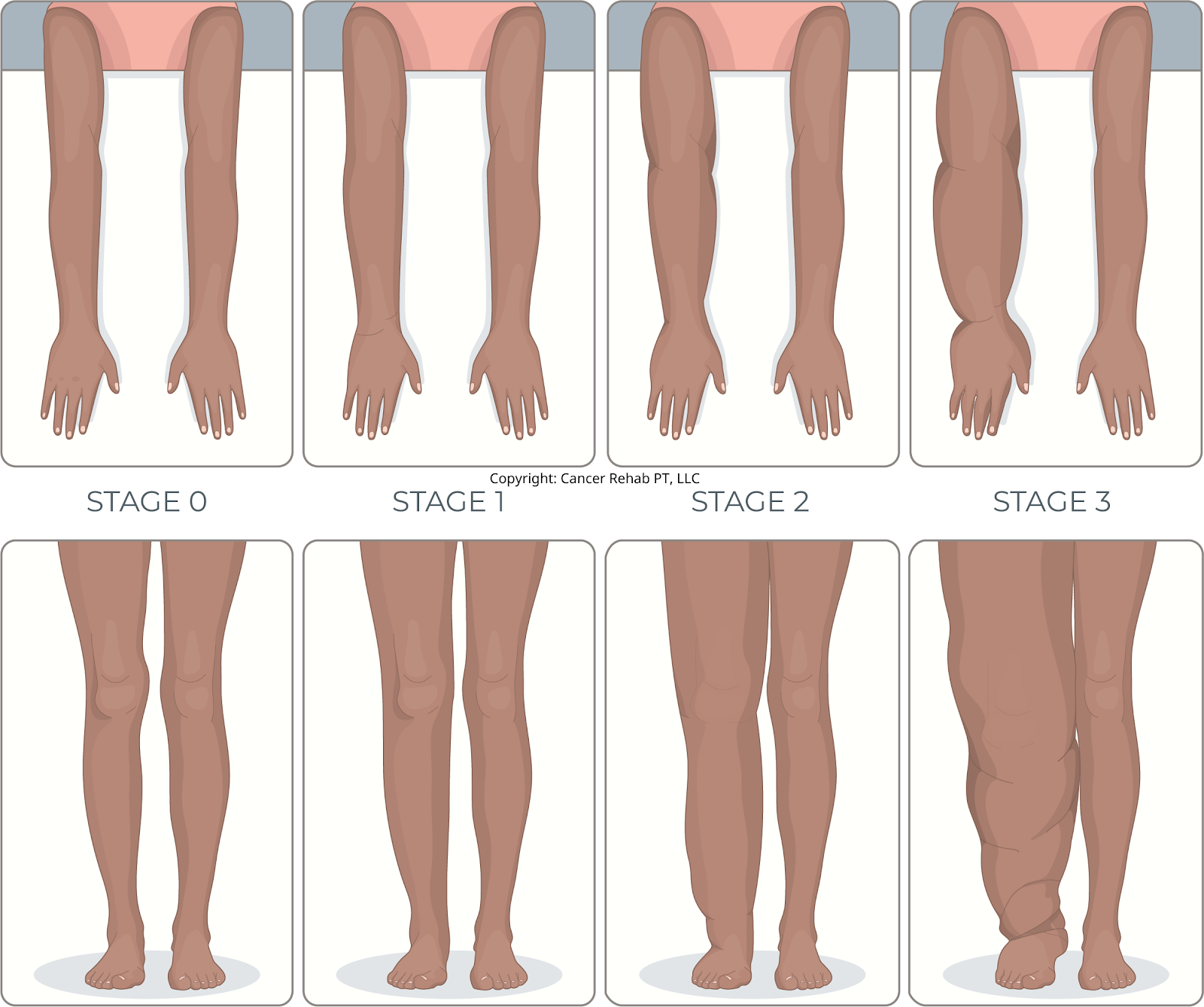
Lymphedema is a chronic condition that causes swelling in the arms, legs, or other parts of the body. There are four lymphedema stages, ranging from Stage 0 (where damage exists but swelling hasn’t appeared yet) to Stage 3 (severe swelling).
It’s often possible to prevent lymphedema from progressing to more severe stages. In my practice as a certified lymphedema therapist (CLT-LANA), I’ve also seen early-stage swelling improve or even go away naturally with proper management and care.
What Is Lymphedema?
Lymphedema is chronic swelling that occurs when your lymphatic system can’t properly drain lymph fluid from your tissues. It can develop in the arms, legs, neck, pelvis, and other parts of the body.
There are two types of lymphedema:
- Primary lymphedema affects people with an inherent lymphatic dysfunction. It’s often present at birth or can develop later in life. It’s very rare.
- Secondary lymphedema develops after your lymphatic system gets damaged. This damage often comes from cancer treatments like lymph node removal, radiation therapy, or surgery, but can also result from infections, injuries, or other medical procedures.
Secondary lymphedema is very common, and researchers estimate that 1 in 30 people live with lymphedema worldwide. This condition doesn’t have a cure, but effective management can reduce or even eliminate swelling and help you maintain an active lifestyle.
What Causes Lymphedema?
Several factors increase your risk of developing lymphedema. Any medical procedure that involves your lymph nodes, whether it’s surgical removal or radiation therapy, can damage your lymphatic system and increase your risk.
Cancer treatment (especially breast cancer treatment) is one of the most common causes of secondary lymphedema.
Other risk factors include infections that affect your lymph nodes, traumatic injuries, burns, surgeries, and certain medical conditions that impact lymphatic function.
There’s no way to predict whether you’ll develop lymphedema, but being aware of your risk and early detection can prevent lymphedema from progressing to more severe stages.
Lymphedema Stages
Lymphedema is classified into four stages, from Stage 0 (earliest changes with no visible swelling) to Stage 3 (severe swelling). It’s important to treat lymphedema no matter the stage.
Stage 0
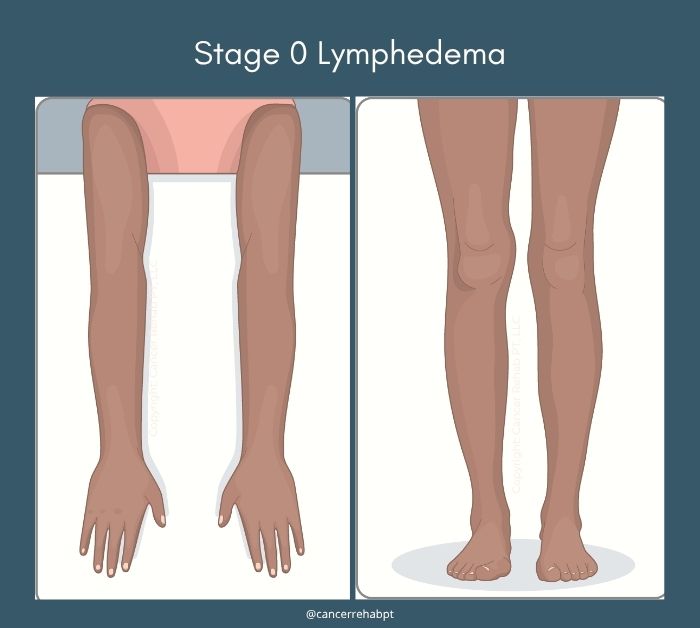
At Stage 0 (also known as the “latent stage”), your lymphatic system has been damaged, but you don’t see any swelling yet. This stage can last months or even years before progressing.
You might still notice subtle changes like a feeling of heaviness in your arm or leg. Some people experience occasional aching or discomfort in the affected area where lymph nodes were removed or damaged.
However, your skin still looks and feels normal, and you can move without any restrictions. Early-stage lymphedema is often reversible with proper treatment.
Stage 1
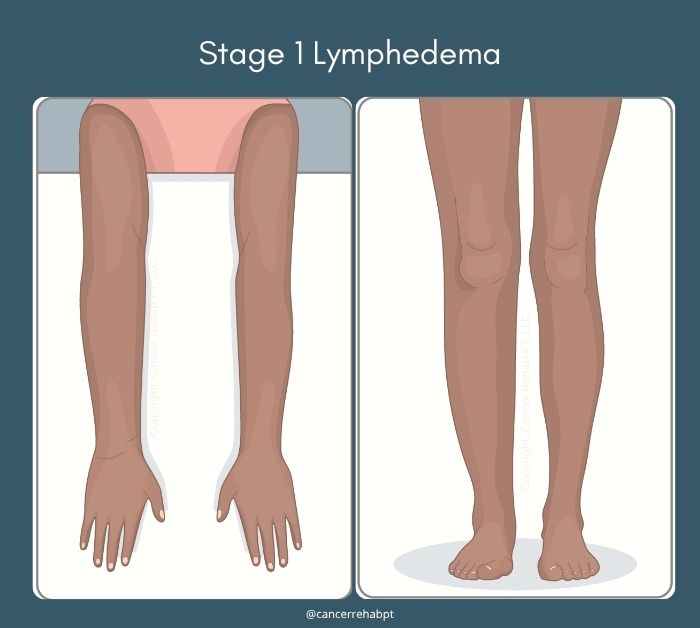
Stage 1 is when swelling first becomes visible, but it’s still considered mild and reversible lymphedema.
The swelling comes and goes. You might notice it more at the end of the day or after an activity, then see it go down overnight or when you rest with your limb elevated.
When you press on the swollen area, it leaves an indent that slowly fills back in (“pitting edema”). If you don’t treat lymphedema at this stage, the swelling will keep getting worse and become harder to manage. Proper diagnosis and treatment are very important to prevent further damage. Compression therapy, exercise, and manual lymphatic drainage are all very effective at this stage and can help keep the swelling down or even naturally reverse it.
Stage 2
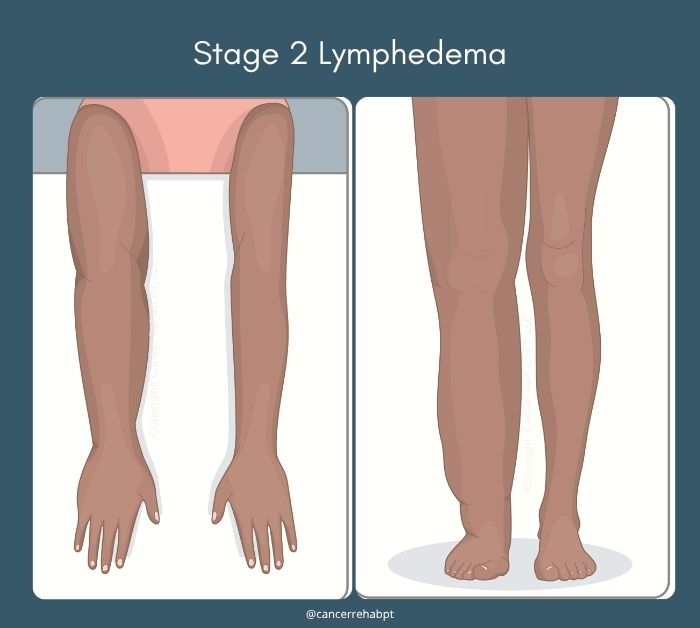
Stage 2 swelling doesn’t go away on its own anymore, even with rest or elevation. The affected arm or leg stays swollen throughout the day and night. It’s known as moderate lymphedema or irreversible lymphedema (because the swelling doesn’t go down on its own).
When you press on the skin, it may not indent as easily, or the indent takes longer to fill back in. You might start to notice your skin feels firmer or thicker than normal.
The swelling becomes more noticeable and may begin to interfere with how clothes fit or how easily you can move the affected limb.
Lymphedema treatment can still help reduce swelling at this stage, but you may not be able to completely get rid of it.
Related Article: What Kind of Doctor Treats Lymphedema?
Stage 3
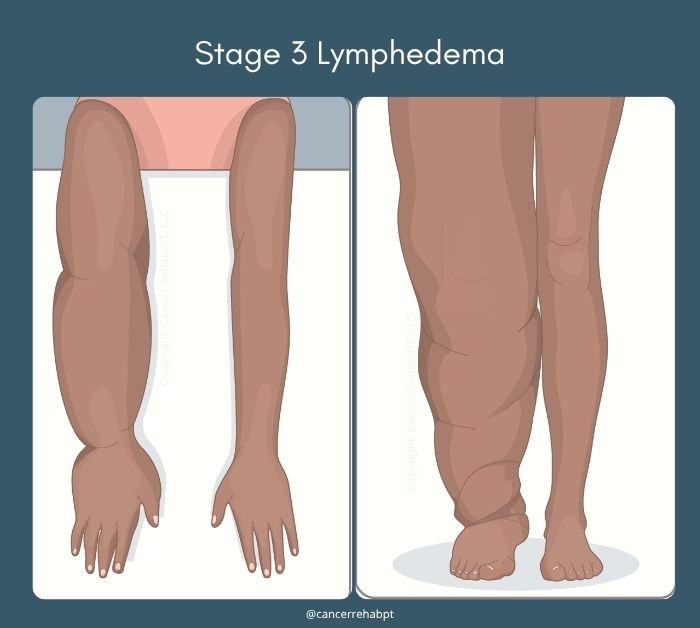
Stage 3 is severe lymphedema, with significant and permanent swelling that changes the shape and size of your limb. Your skin becomes very thick, hard, and may develop a bumpy texture.
The affected area is much larger than normal and doesn’t respond to pressing, the tissue feels firm. Movement becomes more difficult due to the size and weight of the excess fluid.
Without treatment, Stage 3 lymphedema can lead to serious complications like recurring infections (especially cellulitis) and skin breakdown.
Lymphedema Early Stages
The early stages of lymphedema (Stages 0 and 1) are the best opportunities for effective treatment and prevention of progression.
In my practice, the swelling at these stages can become minimal or even be reversed naturally. Even if you’ve lived with mild lymphedema for some time, treatment can make a big difference.
What Is the Most Effective Treatment for Lymphedema?
Once you’ve been diagnosed with lymphedema, you’ll typically work with a certified lymphedema therapist and do a cycle of Complete Decongestive Therapy (CDT).
It’s an intensive treatment stage that combines compression therapy, physical exercise, manual lymphatic drainage, and other treatment options to reduce swelling and improve lymphatic circulation as much as possible.
After completing therapy with your CLT, you’ll transition to lymphedema self-care at home to maintain your progress.
Your routine will typically include:
- Exercise: Physical movement acts as a “pump” for your lymphatic system and helps your lymph vessels and nodes drain excess fluid.
- Manual lymphatic drainage: Gentle massage techniques to encourage lymph flow that you can do at home.
- Compression garments: Special lymphedema products, such as fitted sleeves, stockings, or wraps, that help move fluid out of the affected area.
- Skin care: Proper cleaning and moisturizing to prevent skin infections, which are common with lymphedema.
- Others: Each person is unique and may also benefit from a pneumatic compression pump, vibration plates, or other tools to treat and manage lymphedema
It’s important to experiment with your lymphedema management routine and see what treatment options make the biggest difference for your symptoms. If you’re looking for different forms of exercise, I recommend rebounder workouts and vibration plates for better lymphatic drainage.
How Fast Does Lymphedema Progress?
It varies from person to person. For some people, it can progress slowly over months or even years. For others, the swelling can get worse faster if left untreated.
I have also worked with patients whose lymphedema developed immediately after a bout of cellulitis or a new surgery.
Your progression depends on several factors, including how much damage occurred to your lymphatic system, your overall health, your activity level, and whether you’re taking preventive measures.
Can Lymphedema Go Away?
Lymphedema is a chronic condition that doesn’t go away, but it’s treatable.
In Stage 0 and Stage 1, many people see their swelling reduce or even disappear entirely. However, the underlying lymphatic damage is still there, so you’ll need to continue your self-care routine to maintain these improvements.
If you have more advanced lymphedema, it usually can’t be completely reversed. But even people with Stage 2 or Stage 3 can see big improvements in their swelling and feel much better with proper treatment.
How Bad Does Lymphedema Get?
Without treatment, lymphedema can get pretty severe and make daily life hard.
In the worst cases (Stage 3), your arm or leg can become many times bigger than normal. This makes it difficult to move around, work, exercise, or do everyday things. Your skin can become thick and hard, and it might develop sores or serious infections.
What Is the Life Expectancy with Lymphedema?
Lymphedema doesn’t typically shorten your life expectancy. Most people with lymphedema live normal and full lives when their condition is properly managed.
The main health worry is getting infections like cellulitis, which is a serious skin infection that happens more often in people with lymphedema. Cellulitis can be dangerous if you don’t treat it, but you can prevent it with good skin care. If you do get it, antibiotics can treat it when caught early.
FAQs
How many stages of lymphedema are there?
There are four stages of lymphedema, numbered from 0 to 3. Stage 0 is when your lymphatic system is damaged, but you don’t see any swelling yet. Stage 1 shows mild swelling that comes and goes. Stage 2 has swelling that stays all the time and doesn’t go away with rest. Stage 3 is the most severe, with very large, permanent swelling and thick, hard skin.
Who is a candidate for lymphedema surgery?
No surgery has been proven to fix lymphedema because it’s a chronic condition with no known cure. However, certain procedures, such as lymphaticovenous bypass (LVB or LVA) and Vascularized Lymph Node Transfer (VLNTx), can sometimes help improve symptoms.
Good candidates are typically healthy overall, have realistic expectations, and have exhausted conservative treatments first.
When does lymphedema become an emergency?
Lymphedema becomes an emergency when you develop signs of a serious infection, like cellulitis. Warning signs include a sudden increase in swelling, red streaks on your skin, skin that feels hot to the touch, fever, chills, or flu-like symptoms. You should also seek immediate help if you have severe pain, open wounds that won’t heal, or if your skin starts breaking down. These complications can be dangerous if not treated quickly with antibiotics.
What causes lymphedema to flare up?
It depends on your unique triggers. Infections, injuries, hormonal changes, certain medications, hot or cold weather, and even stress can increase swelling. Over time, you’ll be able to tell which activities make your lymphedema swelling worse and plan better to avoid them. Skipping your lymphedema self-care routine (ex, not wearing compression garments or exercising) can also cause flare-ups.
Can compression garments make lymphedema worse?
Compression garments can make lymphedema worse if they don’t fit properly or aren’t the right type for your condition. Garments that are too tight, too loose, or have the wrong compression level can block lymph flow instead of helping it. Old, worn-out garments that have lost their compression can also be ineffective.
It’s important to get garments that fit properly and replace them regularly. I recommend replacing garments every four to six months.
Is lymphedema life-limiting?
Lymphedema doesn’t have to be life-limiting for most people. With proper management, many people with lymphedema live active, fulfilling lives with minimal restrictions. You might need to make some adjustments to your daily routine and be more careful about certain activities, but you can still work, exercise, travel, and enjoy hobbies. However, lymphedema has a much higher risk of becoming life-limiting without proper treatment.
Managing Lymphedema Symptoms
There are four lymphedema stages, ranging from no visible swelling (Stage 0) to severe swelling that can interfere with daily activities (Stage 3).
However, with consistent treatment, you can improve lymphedema symptoms and live a full life. Especially in the early stages, lymphedema can often cause only minor swelling or even be reversible.
As a certified lymphedema therapist (CLT-LANA), I’ve spent over a decade helping people manage pain and swelling. However, I saw that lymphedema education and care weren’t accessible to everyone who needed them, which is why I started sharing my expertise online.
You can find education & practical resources on how to manage lymphedema in my programs, Lower Body Lymphedema Rehab, Breast Cancer Rehab, or Printable Guides.