Lymphedema in the neck and head causes swelling when your lymphatic system can’t properly drain fluid from these areas. This chronic condition often develops after cancer treatment, but it can also result from infections, injuries, or genetic factors.
Unfortunately, there’s no cure for head and neck lymphedema. However, proper management can make a big difference in your quality of life. Through my work as a certified lymphedema therapist (CLT-LANA), I’ve seen many people with head and neck lymphedema continue living full, active lives.
What Is Lymphedema in the Neck and Head?
With lymphedema in the neck and head, lymph fluid builds up in the tissues of your face, neck, or scalp. Normally, your lymphatic system moves this fluid out, but when it gets damaged or overworked, fluid accumulates and causes visible swelling.
There are two main types of lymphedema:
- Primary lymphedema is genetic and develops because your lymphatic system didn’t form properly. This type is relatively rare and usually appears earlier in life.
- Secondary lymphedema develops after damage to your lymphatic system from surgery, radiation, infection, or trauma.
Most head and neck lymphedema cases I treat in my practice are secondary lymphedema related to cancer treatment.
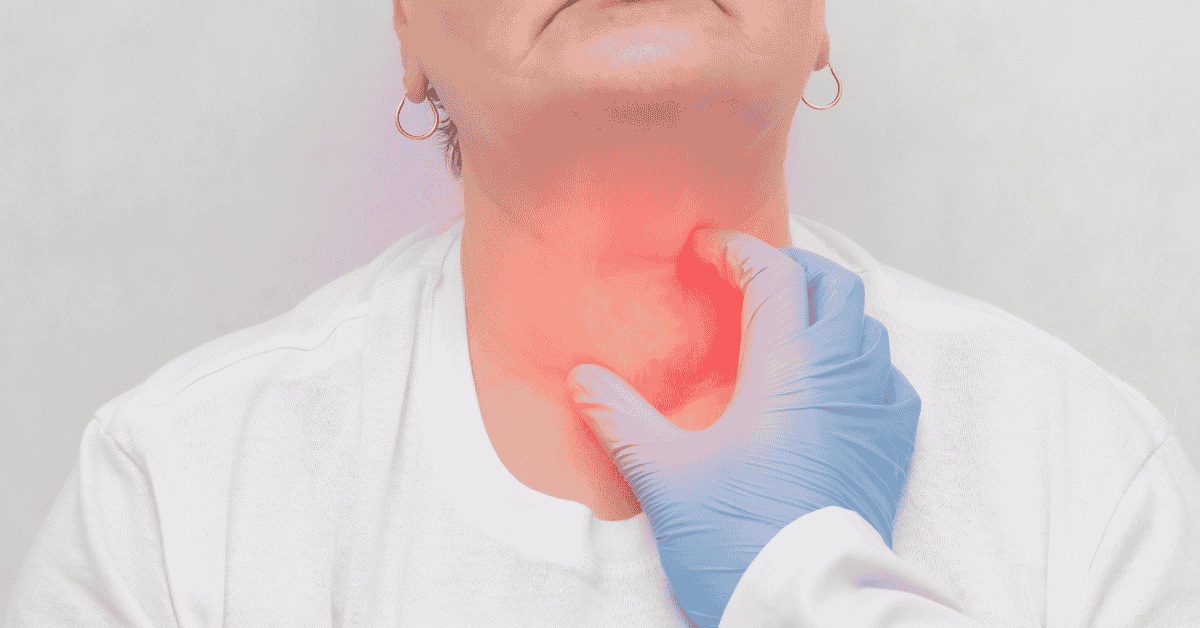
The head and neck region has lymph nodes that filter fluid from your face, scalp, mouth, and throat. When these nodes are removed during surgery or damaged by radiation, your lymphatic system may have a harder time moving fluid like it used to. This leads to swelling.
Lymphedema affects millions of people worldwide. Up to 250 million people globally have this chronic condition, but head and neck lymphedema specifically is relatively uncommon.
Lymphedema in the Neck and Head Symptoms
Head and neck lymphedema can look different from person to person. Common symptoms I see in my patients include:
- Visible puffiness or swelling in your face, neck, chin, or under your jaw
- Tight, heavy, or uncomfortable feeling in the swollen areas
- Swollen eyelids that make your eyes appear puffy or partially closed
- Enlarged lips or swelling inside your mouth affecting your tongue or throat
- Difficulty swallowing, speaking clearly, or breathing through your nose
- Skin that leaves a temporary indent when pressed (early stages) or feels firm and won’t indent (later stages)
- Thickened, leathery skin or changes in skin color
- Reduced range of motion in your neck, making it harder to turn or tilt your head
You may develop lymphedema neck and head swelling on one side, or across your entire face and neck. It can be very uncomfortable or even painful, especially in the later lymphedema stages.
What Can Trigger Lymphedema in the Neck and Head?
Head and neck cancer treatment is the most common trigger for lymphedema in those areas.
Surgery to remove tumors in the head or neck region often requires removing lymph nodes as well, and radiation therapy damages lymph vessels and nodes in the treatment area.
Unfortunately, up to 75% of head and neck cancer patients will develop lymphedema at some point after treatment.
In my clinical experience, this statistic holds true. That said, keep in mind that some people notice swelling almost immediately after head and neck surgery/radiation therapy, and others don’t develop symptoms until months or even years later.
Even though cancer treatment is the leading cause of head and neck lymphedema, other things can damage your lymph system, too:
- Infections in your head, neck, or upper body, such as dental or sinus infections
- Injuries or trauma to your head or neck
- Dental procedures or surgeries
Receiving a lymphedema diagnosis can feel scary, and living with chronic swelling in your head and neck can be really uncomfortable. However, I often remind my patients that proper lymphedema management can help them live a full life with minimal restrictions.
Is Lymphedema in the Neck and Head Serious?
Head and neck lymphedema is a chronic condition that requires ongoing management. Without it, swelling will get worse over time and can lead to serious complications.
The most serious risk is infection.
When lymph fluid builds up in your tissues, it creates an environment where bacteria can grow easily. For example, cellulitis is a common infection in people with untreated lymphedema. This bacterial skin infection causes redness, warmth, pain, and fever. You must treat cellulitis with antibiotics.
Untreated lymphedema can also lead to thickened, hardened skin (called fibrosis), difficulty breathing, reduced mobility in your neck, and problems with daily activities like eating and speaking.
However, these complications are avoidable with consistent treatment and self-care.
Lymphedema in Head and Neck Life Expectancy
Lymphedema doesn’t affect your life expectancy. With proper management, people with head and neck lymphedema live normal, healthy lives.
You don’t have to accept chronic swelling as your new normal.
I’ve worked with many patients who’ve successfully reduced their head and neck lymphedema and kept it under control long-term.
Head and Neck Lymphedema Treatment
The standard treatment for head and neck lymphedema is Complete Decongestive Therapy (CDT). This approach has two phases that use the same core techniques.
During Phase 1, you work with a certified lymphedema therapist.
They’ll do manual lymphatic drainage massage, apply compression bandages or garments, teach you exercises, and help you develop proper skin care habits. This intensive phase typically lasts a few weeks, and the goal is to get the swelling down as much as possible.
Phase 2 is the lymphedema self-care phase.
Once your swelling is under control, you’ll start managing lymphedema at home. Typically, this means using the same techniques your therapist taught you, such as wearing compression garments and doing manual lymphatic drainage.
This maintenance phase is lifelong and keeps your swelling from returning.
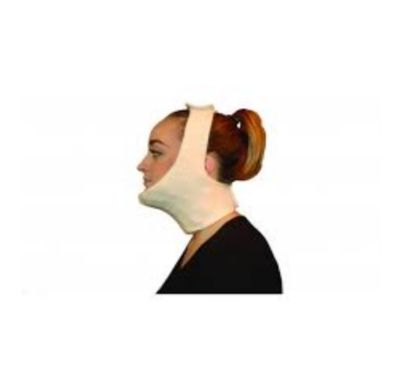
Compression Therapy
Compression therapy is the practice of using special garments or bandages to apply gentle pressure to the swollen areas of your neck or head. This pressure helps move lymph fluid out of your tissues.
For head and neck lymphedema, compression might include face masks, chin straps, or foam padding held in place with soft wraps.
Usually, you’ll wear compression garments daily for several hours or as recommended by your therapist.
If you’re looking for compression options, here are a few garments I’ve seen work well with my patients:
Manual Lymphatic Drainage (MLD)
Manual lymphatic drainage is a massage technique that moves lymph fluid from swollen areas toward working lymph nodes. The massage uses very light pressure and rhythmic movements that follow the direction of lymphatic flow.
For head and neck lymphedema, your therapist will do gentle strokes on your neck, face, and upper chest to redirect fluid away from congested areas.
As you transition to self-care, you’ll learn simple self-massage techniques you can do at home. Here are some helpful guides for you to get started:
Dry Brushing to the Neck and Face for a Healthy Lymphatic System – Digital
Head and Neck Lymphedema Exercises
In general, exercise and staying active help pump lymph fluid through your lymph system by activating your muscles. Even something as simple as going for a walk can be helpful.
Your physical therapist will teach you exercises tailored to head and neck lymphedema, such as neck stretches and shoulder rolls.
That said, your exercise routine doesn’t have to focus only on your head and neck. Virtually all forms of movement are beneficial, so you can try yoga or lymphatic drainage-friendly exercises like vibration plates and rebounder workouts.
Skin Care
Proper skin care is very important for preventing infections in the affected area. When lymph fluid accumulates, your skin becomes more vulnerable to cuts, scratches, and bacterial infections.
The goal is to keep your skin in the head and neck areas clean and well-moisturized.
Use gentle, fragrance-free cleansers and moisturizers, and check your skin regularly for any cuts, rashes, or signs of infection like redness, warmth, or increased swelling. If you do get a cut or scratch, clean it right away.
Good oral hygiene is also important, as dental infections can trigger lymphedema flare-ups.
Healthy Habits
Beyond the core components of CDT, a healthy lifestyle can support lymphedema management and reduce external swelling.
One of the most important things you can do is stay at a healthy body weight.
Excess weight makes it harder for the lymphatic fluid to drain properly, so even modest weight loss can improve your symptoms and lymph flow.
Eating anti-inflammatory foods may also help reduce swelling.
Focus on fatty fish, leafy greens, berries, nuts, olive oil, and whole grains, and avoid processed foods, refined sugars, and fried foods that can increase inflammation.
Learn more about lymphedema diet and how your eating habits can help with symptom management.
Does Neck Lymphedema Go Away?
Neck lymphedema is a chronic condition, which means it doesn’t completely go away on its own. But the fact that it’s chronic doesn’t mean that you’re stuck with swelling forever.
With proper treatment through Complete Decongestive Therapy and self-care, most people can reduce the swelling or even almost completely get rid of it.
In the very early stages, lymphedema can also be reversible. If you’ve had cancer surgery or radiation treatment recently, watch out for lymphedema signs to catch it as soon as possible.
FAQs
Who are the doctors who treat head and neck lymphedema?
Certified lymphedema therapists are the primary professionals who treat head and neck lymphedema. These are physical therapists or occupational therapists who have completed specialized training in lymphedema management and earned their certification (CLT-LANA).
Your treatment team might also include your oncologist or surgeon, who monitors your overall health after cancer treatment, a dermatologist if you develop skin complications, and your primary care physician, who can prescribe antibiotics if you develop an infection.
How to get rid of lymphedema in the neck?
You can’t completely get rid of lymphedema, but you can reduce the swelling through Complete Decongestive Therapy and self-care. Different routines work for different people, but most include a combination of manual lymph drainage, compression therapy, physical exercise, and skin care.
Do you have lymphedema if you have cancer?
Not everyone who has cancer develops lymphedema. However, cancer treatment, especially surgery that removes lymph nodes and radiation therapy, significantly increases your risk. Up to 75% of head and neck cancer patients will develop some degree of lymphedema after treatment. However, catching it early helps prevent severe lymphedema from developing and keeps the swelling minimal.
Physical Therapy Resources for Head and Neck Lymphedema
As a certified lymphedema therapist (CLT-LANA) and doctor of physical therapy, I work with many lymphedema patients, including those dealing with head and neck swelling.
I want you to know that chronic swelling shouldn’t control your daily life, and effective management can dramatically reduce your symptoms and help you feel more comfortable.
At the same time, I understand that seeing a physical therapist in person isn’t always practical. The cost of ongoing appointments adds up, and driving to a clinic multiple times per week can be difficult, especially when you’re already managing a chronic condition.
That’s why I created comprehensive guides to help you with lymphedema management and self-care.
These resources give you the knowledge and techniques you need to take control of your treatment at home: