Although lymphedema is a chronic condition, incorporating lymphedema self-care practices into your daily routine can help you significantly improve your symptoms.
After your lymphedema diagnosis, you may have been told that discomfort is now your new normal. This doesn’t have to be the case. With proper lymphedema treatment and self-care routine at home, you can minimize discomfort and maximize your life.
What Is Lymphedema?
Lymphedema is a chronic condition that occurs when there’s a backup of lymph fluid in certain areas of your body. It leads to swelling in the legs, arms, and other parts of the body, which can interfere with daily activities and be highly uncomfortable.
There are two types of lymphedema: primary lymphedema and secondary lymphedema.
- Primary Lymphedema: Primary lymphedema is a medical condition that occurs when someone is born with a problem in their lymphatic system, causing swelling in parts of their body. It’s very rare.
- Secondary Lymphedema: Secondary lymphedema happens when the lymphatic system gets damaged because of surgery, cancer treatment, radiation treatment, infection, or injury. It’s much more common.
Researchers estimate that up to 250 million people worldwide have lymphedema. While there’s no cure for the condition, there are effective ways to manage it to alleviate discomfort and live a fulfilling life.
What Is Lymphedema Self-Care?
Most people first work with a lymphedema therapist or a lymphedema specialist on Complete Decongestive Therapy (CDT).
Complete Decongestive Therapy is an intensive treatment that combines manual lymphatic drainage, compression bandaging, exercise, and skin care to reduce swelling. The primary objective is to get your swelling down and get you to a place where you can continue lymphedema self-care at home.
Lymphedema self-care is the daily habits and techniques you do at home to manage your swelling, prevent flare-ups, and maintain the progress you made with your lymphedema treatment.
You’ll still probably see your lymphedema specialist once a year or so to check on your progress. How often you need to see your lymphedema therapist depends on whether you have severe swelling or any flare-ups. You’ll also need medical attention if you develop any signs of infection, such as cellulitis.
But when you have a good lymphedema self-care routine, you don’t need treatment as frequently, and your chances of infection are low.
8 Ways to Manage Lymphedema Symptoms at Home
There are a few different ways you can do lymphedema treatment at home to keep your lymphatic system healthy and reduce swelling. In the next sections, you’ll learn about the following lymphedema self-care tools and techniques:
- Compression therapy
- Physical exercise
- Rebounder workouts
- Vibration plates for lymphatic drainage
- Manual Lymphatic Drainage (MLD)
- Skin care
- Dry brushing
- Healthy habits
You can also find more practical education and resources in my programs, Lower Body Lymphedema Rehab and Breast Cancer Rehab.
It’s important to experiment and figure out a lymphedema self-care routine that works for your schedule and is enjoyable for you to do.
If you have to force yourself to follow through with your habits or spend multiple hours on them every day, then it’s going to be hard to stay consistent. Remember that it’s much better to do a little every day than a lot every once in a while. Some self-care techniques might also work for you better than others.

1. Compression Therapy
Compression therapy is one of the most effective ways of treating lymphedema at home. It involves the use of specialized garments, bandages, or pneumatic devices to apply controlled pressure to the affected limb or area of your body.
This pressure helps the weakened or damaged lymphatic vessels move lymph fluid toward healthy lymph nodes for better drainage. It should be supportive and gentle. Avoid wearing garments that are not made for swelling, don’t fit properly, or apply too much pressure that causes a tourniquet.
Choosing Compression Garments
Compression garments come in various forms, including sleeves, stockings, gloves, and bandages.
They are designed to accommodate different areas of the body affected by lymphedema (for example, your arms, legs, or pelvis). You can get garments with different compression levels, ranging from mild to high, depending on how severe the swelling is.
Wearing Compression Garments
The most important thing when it comes to compression therapy and lymphedema self-care in general is to stay consistent. Stick to a regular schedule to keep your swelling under control and prevent lymphedema complications.
It’s also important to follow manufacturer guidelines for washing and caring for your lymphedema products to keep them effective. Proper hygiene helps prevent skin irritation and extends the life of your garments.
I recommended replacing compression garments every four to six months. After months of daily use, compression stockings and sleeves don’t hold the proper amount of stretch to support swelling or edema and should be replaced.
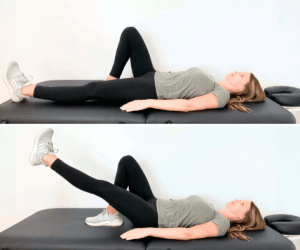
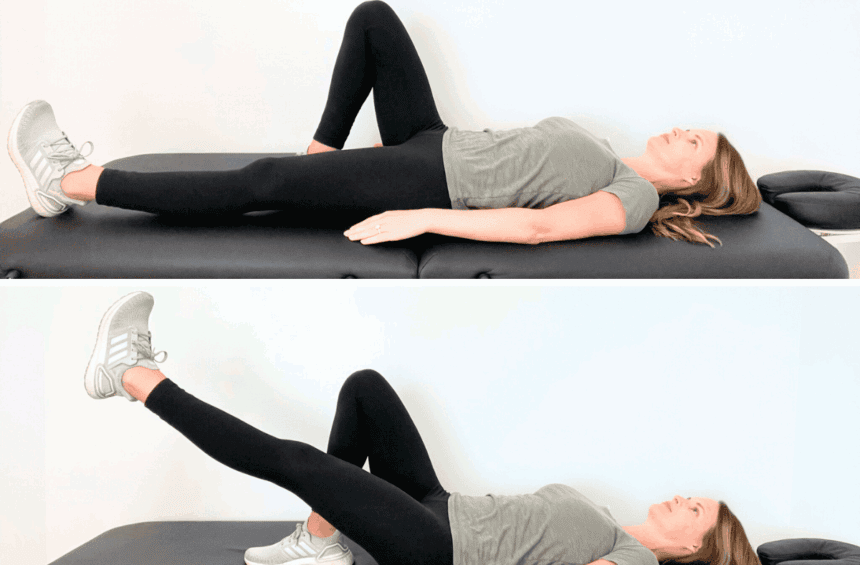
2. Physical Exercise
Exercise is a powerful lymphedema self-care habit that can help you reduce swelling, improve mobility, and feel stronger.
Physical movement stimulates lymphatic flow and muscle contractions, helping fluid flow through lymph nodes and lymph vessels. While it may feel counterintuitive to exercise with lymphedema, consistent physical activity can be highly beneficial:
- Improved lymphatic circulation: Regular physical activity stimulates lymphatic flow and circulation, helping to reduce fluid buildup and alleviate swelling in affected areas.
- Muscle pumping: Exercise encourages muscle contractions, which act as natural pumps and move lymph fluid through the lymph nodes and vessels.
- Joint mobility and flexibility: Lymphedema can make you feel stiff and limit your range of motion, but physical exercise (especially stretching) can help you feel more flexible and comfortable.
- Healthy weight: A regular exercise program, especially when paired with a healthy diet, can help with weight management, increase lymph flow, and improve your quality of life.
- Better mental health: Exercise can boost your mood and reduce stress, which helps you stay more positive and resilient while living with lymphedema.
I encourage those with lymphedema to focus on doing physical exercise that they enjoy. Take regular walks, do yoga, or try swimming: the most important thing is that it should feel good to move. When exercise brings you joy and fulfillment, it’s much easier to stay consistent.
Try my exercises for leg swelling and arm and chest swelling, or join my program, Lower Body Lymphedema Rehab.
Increasing Exercise Intensity
It can be tempting to start exercising a lot right away, but overdoing activities can make lymphedema swelling worse or cause injury. For best results, start with low-impact exercises and gradually increase intensity and duration as tolerated.
Pay attention to changes in swelling, discomfort, or fatigue during and after exercise. If symptoms worsen or persist, stop exercising and consult with your physical therapist.
3. Rebounder Workouts
A rebounder is a small, personal trampoline that you can use for gentle bouncing exercises at home. The soft, rhythmic movement of rebounding creates a pumping action that helps stimulate your lymphatic system without putting stress on your joints.
Rebounder workouts can be a great way to do lymphedema self-care:
- Gentle lymphatic stimulation: The up-and-down movement helps lymph fluid flow through your vessels and toward healthy lymph nodes
- Low-impact exercise: You get the benefits of movement without harsh impact on your joints or risk of injury
- Improved circulation: The bouncing motion encourages blood circulation and reduces fluid buildup
- Easy to do at home: You can bounce for just 5-10 minutes a day in your living room
Many people find rebounding enjoyable, which makes it easier to stick with.
4. Vibration Plates
Vibration plates are platforms that produce gentle vibrations while you stand or exercise on them. The vibrations create muscle contractions throughout your body, which can help stimulate lymphatic flow and reduce swelling.
This is a relatively new form of exercise, but a couple of different studies have already found that vibration plates can be beneficial for your lymph system.
These findings are promising, but it’s not a magic cure. Some people find vibration plates very helpful, and others prefer other forms of exercise.
5. Manual Lymphatic Drainage (MLD)
Manual Lymphatic Drainage (MLD) is a gentle massage technique that helps stimulate the natural flow of lymphatic fluid in your body. To do MLD, you need to apply light pressure with your hand to brush and stretch your skin.
The benefits include:
- Better fluid flow: MLD encourages stagnant excess fluid to move toward functional lymph nodes, helping to reduce fluid buildup and swelling.
- Stronger immune system function: MLD’s manipulation of lymph vessels and nodes may help improve your body’s ability to fight infections and stay healthy.
- Scar tissue management: If you had surgery or radiation therapy (for example, for breast cancer treatment), MLD can help soften and mobilize scar tissue so that it heals better.
If you want to try self-massage techniques at home, make sure your healthcare provider (such as your lymphedema therapist) clears you first. If you’re looking for practical resources, try my Both Legs Manual Lymphatic Drainage Guide or Both Arms Manual Lymphatic Drainage Guide.

6. Skin Care
Lymphedema poses risks to your skin and barrier function. Chronic swelling can lead to skin changes such as thickening, hardening (fibrosis), and an increased risk of infection, but a skincare routine can prevent skin breakdown and support your lymph system.
Here’s how to take care of your skin when living with lymphedema:
- Gentle cleansing: Use mild, fragrance-free cleansers and lukewarm water to wash your skin daily, paying close attention to swollen areas and skin folds. Avoid harsh soaps or scrubbing, as they can strip the skin of its natural oils and make the dryness and irritation worse.
- Moisturize: Hydrate your skin regularly to prevent dryness and cracking, which can serve as entry points for bacteria and increase the risk of infection. You can buy a moisturizer at your local store or use a natural option like coconut oil.
- Protect your skin: Minimize your risk of skin injury by wearing protective clothing, avoiding tight-fitting garments or accessories, and just generally protecting vulnerable areas of your skin from trauma. You should wear gloves when gardening and use insect repellent.
- Nail and foot care: Keep your nails trimmed short and smooth to reduce the risk of accidental scratches or cuts that can lead to infection. Try to avoid getting blisters and other common foot injuries.
- Avoid sunburn: Protect your skin from the sun with protective clothing and broad-spectrum sunscreen with a high SPF to keep your skin healthy.
In general, be very careful with your skin. Try to avoid any activities that may result in scratches or cuts, such as shaving underarms and walking barefoot, but, of course, you can’t protect your skin from everything. If you do get injured, even if it’s just a small skin scrape, take care of it right away.
7. Dry Brushing
Dry brushing is a technique where you use a natural bristle brush to gently brush your skin in long, sweeping motions toward your lymph nodes. This simple practice can help stimulate lymphatic flow and reduce fluid buildup.
It takes just 5 to 10 minutes and fits easily into your morning or evening routine.
8. Healthy Habits
Your lymphatic system will benefit from healthy habits, such as drinking enough water, eating nourishing whole foods, and stress management. It’s especially important to stay at a healthy weight because excess fat can put additional pressure on your lymphatic system and make the swelling worse.
It’s important to:
- Drink plenty of water throughout the day
- Include fruits, vegetables, lean proteins, and healthy fats in your diet
- Reduce foods high in sodium, sugar, and artificial ingredients
- Get good sleep to help your body recover and reduce inflammation
You don’t have to change everything at once. Small, consistent changes can add up to big improvements in how you feel and how much swelling you experience.
Building Your Lymphedema Self-Care Toolbox
Lymphedema self-care is a personal journey that requires patience and a willingness to experiment with different treatment options.
Lymphedema manifests differently in each person, and there’s no one-size-fits-all solution. However, there are different tools available to you that you can use to build a routine that works for you.
The most important thing is to stay positive and remember that life without swelling and limitations is possible. You may have been told that you have to accept your new normal after a lymphedema diagnosis, but that’s not true.
There are self-care practices, techniques, and exercises that can improve your quality of life and help you get back to doing things you love.
Try different approaches and keep track of what works best for your body. Give each new tool at least 3 to 4 weeks to see if it’s making a difference in your symptoms. Over time, you’ll build a personalized toolbox of lymphedema self-care practices that help manage your swelling and make you feel your best.
What Causes Lymphedema to Flare Up?
Lymphedema is a chronic disease, and it’s possible to experience sudden flare-ups of swelling and discomfort in affected areas. Flare-ups can be frustrating, but understanding potential triggers can help you be prepared and minimize their impact with a self-care routine.
Some potential triggers for lymphedema flare-ups include:
- Injury or trauma: Cuts, burns, insect bites, or blunt force trauma can disrupt the flow of lymphatic fluid and increase swelling in affected areas.
- Infection: Bacterial or fungal infections (for example, cellulitis) can cause inflammation and compromise lymphatic function, leading to flare-ups.
- Surgery or medical procedures: Procedures like lymph node removal or radiation therapy can disrupt lymphatic flow and worsen existing symptoms.
- Inactivity or immobility: Lack of movement can decrease lymph circulation and contribute to fluid buildup, resulting in flare-ups.
- Heat and humidity: High temperatures and humidity levels can increase fluid retention, leading to more swelling.
- Hormonal changes: For some people, hormonal fluctuations during their menstrual cycle, pregnancy, or menopause can trigger flare-ups.
- Stress: Feeling stressed or anxious can affect lymphatic function and fluid retention in some people.
- Diet and nutrition: Eating too many processed foods or foods high in sodium can contribute to fluid retention and lead to flare-ups.
- Tight clothes or garments: Clothing or jewelry that is too restrictive can block lymphatic flow and make swelling worse. Keep in mind that wearing specialized compression garments is different from wearing tight clothes
- Being on an airplane: Traveling to high altitudes or air travel can affect fluid balance and circulation, potentially causing flare-ups.
The triggers above don’t affect all people with lymphedema. Figuring out what your unique triggers are and developing a strong self-care routine can help you minimize flare-ups and feel more confident.
Lymphedema Self-Care FAQs
How to prevent lymphedema from progressing?
Lymphedema treatment and self-care will help you prevent lymphedema from getting worse. In some cases, it’s even possible to naturally reverse early-stage lymphedema. Lymphedema treatment typically means Complete Decongestive Therapy (CDT) with a lymphedema physical therapist, followed by a self-care routine that you’ll continue to do at home. It can include wearing compression garments, exercising, taking care of your skin, and other important management techniques.
What is the life expectancy of someone with lymphedema?
People with lymphedema can live normal and full lives, but it’s important to manage your lymphedema symptoms and prevent skin infections. Lymphedema itself doesn’t affect your life expectancy, but serious infections like cellulitis can become very dangerous, especially when left untreated. The biggest concern with lymphedema is reducing swelling and maintaining a good quality of life, not life expectancy.
What is the best position to sleep in with lymphedema?
Elevating the affected arm, leg, or body area can help reduce swelling while you sleep. If you have leg lymphedema, prop your legs up with pillows. For arm lymphedema, try sleeping on your back with your arm elevated on a pillow. Generally speaking, find a comfortable position that keeps the swollen area higher than your heart.
Does drinking more water help with lymphedema?
Drinking more water can potentially help with lymphedema management, but it’s not a direct treatment for the condition. Adequate hydration is essential for most body functions and can indirectly positively influence your lymphatic system.
What is the most effective treatment for lymphedema?
Lymphedema manifests differently in different people, and no one approach works well for everybody. The good news is that there are many treatment options available, including compression therapy, physical exercise, and Manual Lymphatic Drainage (MLD). It’s important to build an at-home lymphedema management routine that works for your symptoms, and that usually takes some experimenting to see what your body responds to.
Are there any home remedies for lymphedema?
There are, unfortunately, no home remedies that can cure lymphedema, but there are several self-care practices that help manage symptoms and improve your quality of life. Compression garments, elevation, exercise, and skin care are just some examples of lymphedema home treatment options.
Can lymphedema go away with exercise?
Exercise can’t cure lymphedema, but it’s one of the best ways to manage it. Building a consistent exercise routine can improve your lymph flow, minimize swelling, and help you get back to doing things that you enjoy. Exercise, together with a solid lymphedema self-care routine, can make your swelling pretty minimal, especially in the early stages of lymphedema.
Lymphedema Self-Care Resources
Unfortunately, regularly seeing a lymphedema therapist isn’t always accessible due to location, cost, or long wait times. Or, sometimes, you complete a cycle of Complete Decongestive Therapy (CDT) but feel lost about what to do at home to keep managing your swelling.
As a certified lymphedema therapist (CLT-LANA), I’ve created practical resources using my clinical expertise to make effective lymphedema treatment and self-care more accessible to everyone.
You can find lymphedema self-care education and practical resources in Lower Body Lymphedema Rehab, Breast Cancer Rehab, and my Digital Guides.