What does lymphedema pain feel like? If you’re dealing with swelling and experiencing discomfort, you might be wondering if these are lymphedema symptoms, especially if you went through cancer treatment in the past.
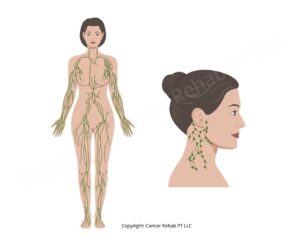
Lymphedema happens when lymph fluid builds up in your arm, leg, or other part of the body after your lymphatic system is damaged, causing swelling and a range of other symptoms, including pain.
There’s no cure for lymphedema, but treatment can effectively manage your symptoms and reduce or even eliminate the pain that sometimes comes with the swelling.
What Is Lymphedema?
Lymphedema is swelling that occurs when your lymphatic system can’t drain fluid from a certain part of your body, most commonly your arm or leg. That said, you can also develop lymphedema in your genital area, neck, or other areas.
The most common type is secondary lymphedema, which develops after cancer treatment or another injury damages your lymphatic system. This often happens after breast cancer treatment, but it can occur with other cancers, too.
When lymph nodes are removed during surgery or damaged by radiation therapy, the remaining lymph vessels can’t always handle the fluid load, and it backs up in your tissue.
Primary lymphedema is inherited and more rare, affecting about 1 in 100,000 people and accounting for less than 10% of lymphedema cases in the US.
Lymphedema causes several symptoms:
- Swelling in your arms, legs, chest, or other affected areas
- Heaviness or tightness in the affected limb or area
- Reduced range of motion
- Aching, discomfort, or pain
- Skin changes like thickening or hardness
If you’ve had lymph node removal or radiation therapy as part of your cancer treatment, you’re at risk of developing lymphedema. It can appear weeks, months, or even years after treatment ends.

Does Lymphedema Cause Chronic Pain?
Yes, lymphedema can cause chronic pain in the affected area, but not everyone experiences it. The pain can range from mild discomfort to more persistent aching that affects your daily life. It’s more common with more severe swelling.
What Does Lymphedema Pain Feel Like?
In my practice as a certified lymphedema therapist, most people describe lymphedema pain as a dull, constant ache or a feeling of heaviness and pressure in the affected area.
Your arm or leg might feel tight and uncomfortable, like it’s being squeezed.
Some people feel a burning or tingling sensation, and the pain can get worse as the day goes on or when you’re experiencing a lymphedema flare-up.
The discomfort comes from the lymphatic fluid pressing on your tissue and the stretching of your skin as swelling increases.
In the more advanced stages of lymphedema, the accumulated fluid can put pressure on nerves, creating more pain or numbness.
That said, lymphedema pain responds well to treatment. When you reduce the swelling through Complete Decongestive Therapy (CDT) and maintain it with self-care at home, the pressure on your tissue decreases, and the pain typically improves a lot.
Learn more about physical therapy for lymphedema.
Getting a Lymphedema Diagnosis
If you’ve had cancer treatment that included lymph node removal or radiation therapy and you’re noticing pain, heaviness, or swelling in the affected area, contact your doctor or ask for a referral to a certified lymphedema therapist.
Getting an early diagnosis is very important because lymphedema treatment is most effective in the early stages.
A lymphedema therapist will measure the affected area and compare it to your other limb or to baseline measurements if you have them. They’ll ask about your symptoms, including when you first noticed the pain and what makes it better or worse. The diagnosis is usually clinical, based on your history of cancer treatment, physical examination, and measurements.
Lymphedema doesn’t resolve without treatment, so even if you’re not sure whether what you’re feeling is lymphedema or something else, it’s worth having it evaluated.
How Do I Get Rid of Lymphedema Pain?
There’s no separate treatment specifically for lymphedema pain.
Instead, treating the lymphedema itself reduces the swelling that’s causing your pain. When the fluid buildup decreases, the pressure on your tissue eases, and the discomfort typically improves.
Here’s what lymphedema treatment includes:
Compression Therapy
Compression therapy is one of the most effective ways to manage lymphedema symptoms, including pain. It uses special garments and bandages to apply consistent pressure to your affected area. This pressure helps move excess fluid out of the swollen tissue and back into the lymphatic circulation.
Your lymphedema therapist may use compression bandages to wrap your limb, and you will also likely have to wear compression garments, such as sleeves or stockings, to maintain your progress.
For lymphedema pain specifically, compression provides relief by reducing the fluid pressing on your tissue and nerves. Many people notice that the heavy, achy feeling improves once they start wearing compression regularly.
Here are my favorite compression garments to help with painful swelling:
Exercise
Movement helps pump fluid through your lymph system. When your muscles contract during exercise, they squeeze the lymphatic vessels and encourage fluid to drain. This reduces swelling and relieves the pressure that causes pain.
Low-impact and regular movement works best for lymphedema.
Walking, swimming, and yoga are great options for most people, and your lymphedema therapist can teach you PT exercises to target lymph drainage in your affected area.
I often recommend vibration plate exercises and rebounder workouts to my patients because they create rhythmic movement that stimulates your lymph flow and helps remove excess fluid. At the same time, they’re gentle enough to do even if you’re experiencing lymphedema pain.
I also have helpful guides that walk you through physical therapy exercises you can do at home:
Manual Lymphatic Drainage
When your lymphatic system develops swelling, manual lymphatic drainage massage, or MLD, can help move lymph fluid using very light and rhythmic strokes in specific patterns.
Your lymphedema specialist will most likely do MLD during your treatment sessions, and you can also learn to do this massage yourself at home.
By manually moving the fluid toward areas of your lymphatic system that still work properly, you reduce the pressure and stretching in the affected tissue. Many people feel immediate pain relief after an MLD session and less visible swelling.
Learning how to do MLD gives you a tool to manage pain flare-ups at home. When you notice increased discomfort, you can use the technique to ease the pressure.
If you want to learn, you can follow these guides:
Complete Decongestive Therapy (CDT)
Once you’re diagnosed with lymphedema, you’ll likely start Complete Decongestive Therapy.
CDT is the gold standard treatment for lymphedema, including lymphedema pain.
At first, you’ll see a certified lymphedema therapist several times a week. They’ll use manual lymphatic drainage, compression bandaging, exercises, and skin care to make your swelling and pain go down as much as possible.
Then, you’ll continue to do lymphedema self-care at home. Typically, this means wearing compression garments, doing physical therapy exercises and MLD, and taking care of your skin to keep your swelling under control.
Most people find that once they’ve gone through the intensive phase and learned how to manage their lymphedema at home, their pain stays manageable as long as they keep up with their routine.
While you can’t cure lymphedema, treatment can help you successfully manage most symptoms, even with severe lymphedema.
Does Lymphedema Pain Ever Go Away?
For many people, lymphedema pain improves or even goes away completely with proper treatment. Some people continue to experience mild discomfort even with good lymphedema management, but it’s typically much more manageable than before treatment.
That said, it’s important to stay consistent with your self-care routine.
When swelling is controlled, pain usually stays controlled, too. But if you let your lymphedema management slip (for example, skipping compression or not doing your exercises), the swelling can increase again, and the pain often returns with it.
When Does Lymphedema Pain Become Dangerous?
Lymphedema pain becomes dangerous when it’s accompanied by signs of infection.
If you notice sudden, rapidly worsening pain along with redness, warmth, fever, or chills, you need medical attention right away.
These are symptoms of cellulitis, a serious bacterial infection that can develop in lymphedema-affected areas.
Cellulitis requires immediate treatment with antibiotics, so don’t wait to see if it gets better on its own. Untreated cellulitis can spread through your bloodstream and become life-threatening.
Learn more about when lymphedema can become dangerous.
FAQs
What is the best painkiller for lymphedema?
I don’t usually recommend taking a painkiller for lymphedema. Over-the-counter pain relievers like Tylenol or Advil may help manage lymphedema pain, but they don’t address the underlying cause. Lymphedema should be treated. When you reduce swelling through compression, exercise, and manual lymphatic drainage, the pain typically improves without medication.
If you’re taking pain relievers regularly for lymphedema discomfort, that’s a sign that your lymphedema isn’t well-controlled and you need better treatment.
Is a heating pad good for lymphedema?
No, I don’t recommend heating pads for lymphedema because they can often make the swelling worse. The same applies to hot tubs, saunas, hot baths, and prolonged sun exposure. In general, temperature therapy (hot or cold) isn’t a good option for lymphedema.
How would you describe lymphedema pain?
Most people describe lymphedema pain as a deep and dull ache or heaviness. You shouldn’t feel sharp or stabbing pain. The pain often includes a sensation of fullness, and you might also feel tingling, burning, or numbness in the affected area.
Get Support with Lymphedema Pain and Other Symptoms
As a certified lymphedema therapist (CLT-LANA) and oncology physical therapist, I created accessible programs and resources to help people manage lymphedema and live a full life with minimal limitations.
In my practice, I see many people who didn’t have access to a physical therapist before, so they lived with swelling, pain, and discomfort for months or even years without guidance.
If you’re looking for evidence-based resources to help manage your symptoms, try these:
- Lower Body Lymphedema Rehab: For managing leg, foot, and lower body lymphedema with exercises and self-care techniques
- Breast Cancer Rehab: For recovery after breast cancer surgery or treatment, including lymphedema prevention and management
- Digital Exercise Guides: Step-by-step manuals for manual lymphatic drainage and PT exercises you can do at home
These resources make professional-level lymphedema care accessible to either supplement your sessions with your PT or to help you build a lymphedema self-care routine at home.