Lymphedema in men after breast cancer treatment happens when lymph fluid builds up in your chest, arm, or surrounding tissue after surgery or radiation damages your lymphatic system.
Most people associate both breast cancer and lymphedema with women, but men face the same risks and complications when it comes to developing lymphedema after breast cancer treatment.
As a certified lymphedema therapist (CLT-LANA) and oncology physical therapist, I see how often lymphedema gets overlooked in general. But when you’re a man who’s had breast cancer, finding support and accurate information becomes even more difficult.
Here’s what you need to know about lymphedema symptoms, treatment, and how to manage your swelling so you can live a full and active life.
What Is Breast Cancer-Related Lymphedema?
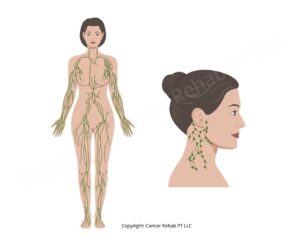
Lymphedema develops when your lymphatic system can’t properly drain fluid from the affected area. For breast-cancer related lymphedema, this usually means swelling in your chest or arm.
Your lymphatic system is a network of vessels and lymph nodes that move fluid throughout your body and filter out bacteria and waste.
When lymph nodes are removed or damaged during cancer treatment, the remaining pathways can’t always handle the fluid load, and it backs up in your chest or arm.
Male breast cancer accounts for approximately 1% of all breast cancer diagnoses. This rarity means less public awareness and often a sense of isolation when you’re trying to find help.
But when it comes to your lymphatic system, there’s no difference between men and women. Your body works the same way, and lymphedema carries the same risk regardless of your sex.
Lymphedema in men after breast cancer isn’t discussed as widely because male breast cancer is rare, not because the condition or its risk factors are different.
In other words, as a man with breast cancer, you’re as likely to develop lymphedema after treatment as a woman with breast cancer.
Learn more about the 5 things they never tell you about life after cancer.
How Common Is Lymphedema After Breast Cancer Surgery?
Lymphedema is one of the most common complications after breast cancer treatment.
Roughly 20% of people will develop arm lymphedema when their treatment includes lymph node surgery and radiation therapy to the lymph nodes.
This applies whether you’ve had an axillary lymph node dissection (where multiple lymph nodes are removed) or a sentinel lymph node biopsy (where only one or a few nodes are taken out and examined).
In my clinic, I see men weeks, months, or even years after their sentinel node biopsy or lymph node removal. Some notice swelling right away, and others develop it gradually. Both patterns are normal.
The risk of lymphedema increases with the number of lymph nodes removed and whether you received radiation therapy.
If you had both an axillary lymph node dissection and radiation to that area, your individual risk may sit at the higher end of that 20% range. A sentinel lymph node biopsy alone carries a lower risk, but it’s still possible to develop lymphedema even when only a small number of nodes were taken out.
Learn how you may be able to prevent lymphedema and lower your risk.

What Does Lymphedema After Breast Cancer Feel Like?
Lymphedema symptoms can start subtly.
Many of the men I work with tell me they first noticed their shirt sleeve feeling tighter on one side, or their chest feeling heavy after a long day.
Common lymphedema symptoms include:
- Swelling in your arm, chest, or shoulder on the treated side
- A feeling of heaviness or fullness
- Tightness in your skin or reduced flexibility
- Aching or discomfort that gets worse with activity or heat
- Clothing that suddenly feels too tight
- Skin that feels harder or thicker than it used to
In the early stages of lymphedema, the swelling might come and go.
You could wake up feeling fine and notice puffiness by evening, especially if you’ve been active or spent time in hot weather. Or you might have mild swelling that stays constant.
Beyond the physical symptoms, lymphedema can bring up difficult emotions.
For many men, it’s a visible reminder of cancer treatment that they want to move forward from. Most importantly, lymphedema is a chronic condition that you’ll need to manage long-term, which can feel frustrating or overwhelming, especially after going through breast cancer treatment.
But lymphedema after breast cancer is manageable.
In the early stages, swelling can sometimes reduce significantly or even reverse with proper treatment. That said, it’s important to catch the condition early and start care right away for the best results.
Once lymphedema progresses to severe swelling, it becomes more difficult to manage. However, physical therapy for lymphedema is effective even in later stages.
Lymphedema Treatment
Lymphedema treatment has two main phases: Complete Decongestive Therapy (CDT) and long-term self-care.
CDT is the intensive phase.
You work with a certified lymphedema therapist, often several times a week, to reduce your swelling as much as possible. The treatment will typically include:
- Compression therapy
- Physical therapy exercises
- Manual lymphatic drainage
- Skin care
The goal is to get your swelling down and teach you how to manage lymphedema at home.
Once your swelling has reduced, you move into the lymphedema self-care phase.
This is where you maintain your progress at home using the techniques you learned during CDT. Most men I work with find that once they understand the routine, it fits into their daily life without taking over and helps them keep their swelling under control.
What Are the Best Ways to Reduce Swelling with Lymphedema?
Compression Therapy
Compression therapy uses garments or bandages to apply gentle and consistent pressure to your affected arm, chest, or another area. This pressure helps push lymph fluid out of the swollen tissue and back into circulation.
During the intensive CDT phase, your therapist will use compression bandaging, with layers of foam and short-stretch bandages wrapped around your arm. For chest swelling, I’ll often recommend a compression shirt or tank, sometimes with swell pads inserted for extra support in specific areas.
Once your swelling has reduced, you’ll often transition to compression garments. These are sleeve-like pieces that fit your arm, or vests and compression shirts that cover your chest and shoulder area.
Your therapist will measure you and help you find garments that fit properly, because poorly fitted compression won’t work as well and can be uncomfortable.
For male patients specifically, options can be more limited. I’ve found that compression tanks or shirts combined with swell pads can work well, though finding the right combination often takes some trial and error.
Some patients have also had success with gynecomastia compression garments, particularly when combined with foam pads underneath for additional pressure. It’s worth noting that the trunk and chest don’t need as much compression as an arm or leg does, so a lower compression level may be enough.
Here are the brands I recommend for my patients as a certified lymphedema therapist: Esteem Apparel Original Men’s Chest Compression Tank and MARENA MV Stage 1 Men’s Adjustable Sleeveless Compression Vest.
Exercise
Moving your body might sound simple, but it’s one of the most effective tools you have for managing lymphedema. When your muscles contract during exercise, they help push fluid through your system.
Virtually any form of physical activity supports lymph drainage.
Staying active in general matters, so walking, swimming, cycling, or any exercise you enjoy will help. But you’ll also benefit from more targeted exercises that focus on lymphatic drainage.
Two types of exercise I often recommend to my patients are vibration plate workouts and rebounder exercises.
Both create rhythmic movements that stimulate lymph flow without putting stress on your joints or requiring intense effort.
That said, the best exercise for lymphedema is exercise that you can stick to doing regularly.
It’s important to keep your lymph fluid moving, so try to do some form of physical exercise every day, even if it’s just for a few minutes.
If you don’t know where to start, I have helpful guides with exercises for lymphedema that you can do at home:
Manual Lymphatic Drainage
Manual lymphatic drainage (MLD) is a massage technique that moves lymph fluid out of swollen areas and redirects it to parts of your lymphatic system that work.
MLD uses very light and rhythmic strokes in specific patterns designed to encourage fluid to flow in the right direction.
Your lymphedema therapist will perform MLD as part of your CDT sessions, but you can also learn to do MLD at home as part of your self-care routine. In my opinion, it’s one of the most valuable skills you’ll learn during treatment.
If you want to learn how to do MLD at home, you can use these guides:
Skin Care
Skin care is very important when living with lymphedema because the condition compromises your immune system in the affected area. With the fluid buildup, your body has a harder time fighting off bacteria and infections.
Even small cuts, scrapes, or irritations can turn into serious infections like cellulitis, which require antibiotics and sometimes a hospital stay.
Here are a few tips to protect your skin and reduce your risk of complications:
- Moisturize daily to prevent dry and cracked skin
- Clean any cuts or scrapes immediately
- Avoid injections, blood draws, or IVs in your affected arm when possible
- Use sunscreen to prevent burns on the affected area
- Wear gloves when doing yard work or other activities that could cause cuts or scrapes
If you get a cut or another injury, watch for redness, warmth, or sudden increased swelling. These symptoms can mean an infection, and it’s important to get treatment for it as soon as possible.
Other Treatments
Compression therapy, exercise, manual lymphatic drainage, and skin care are all parts of CDT, which is the gold standard treatment for lymphedema.
But there are also additional treatment options that can support your care:
- Pneumatic compression devices are machines with inflatable sleeves that wrap around your arm or chest and rhythmically squeeze to move lymph fluid
- Lymphedema surgery includes procedures like lymph node transfer or lymphovenous bypass that create new drainage pathways
- GLP-1 medications can help with weight loss, which typically improves lymphedema symptoms by reducing limb volume
None of these options, including surgery, cure lymphedema. But they’re tools that can help manage it together with your core treatment plan.
In my practice, I encourage men to build their own lymphedema care toolbox. Try different approaches and see what works best for your body, since no two people are the same.
What Happens If Lymphedema Is Left Untreated?
Untreated lymphedema gets worse over time.
The swelling will increase, and it may become difficult to move your arm, which can create inconveniences in your daily life.
Simple tasks like lifting objects, getting dressed, or staying active become harder. Overall, untreated lymphedema can significantly lower your quality of life and prevent you from doing the things you love.
Another big concern is the infection risk. When lymph fluid sits in your tissue for long periods, it creates an environment where bacteria can thrive.
You may develop cellulitis, a serious skin infection, which requires antibiotics and, when not treated on time, can become life-threatening.
Each infection can damage your lymphatic system further, creating a cycle where your lymphedema keeps getting worse and your infection risk keeps increasing.
Overall, managing lymphedema early is far easier than dealing with advanced swelling and repeated infections later.
Learn more about the dangers of untreated lymphedema.
What Kind of Doctor Treats Lymphedema?
Lymphedema is typically treated by a certified lymphedema therapist (CLT), who is usually a physical therapist or occupational therapist with specialized training in lymphedema management.
Your oncologist or primary care doctor can refer you to a CLT in your area.
Not all physical therapists have lymphedema training, so make sure that you’re working with someone who has the proper credentials (CLT-LANA or similar certification).
Learn more about the doctors who treat lymphedema.
What Is the Life Expectancy with Lymphedema?
Lymphedema doesn’t shorten your life expectancy. There’s no cure, and you’ll need to manage the condition for the rest of your life, but treatment can reduce swelling and improve your quality of life.
Most people with lymphedema live a normal lifespan.
The only time lymphedema can impact life expectancy is when it’s left untreated and leads to serious infections. Cellulitis and other bacterial infections need prompt treatment with antibiotics. If ignored, these infections can spread through your bloodstream and become life-threatening.
Learn more about lymphedema life expectancy.
FAQs
How quickly does lymphedema progress?
Lymphedema usually progresses gradually. You may notice mild swelling that stays stable, or it may start to increase slowly. Catching lymphedema early gives you the best chance of managing it well. In the early stages, treatment is most effective, and in some cases, you can even reduce swelling to the point where it’s no longer visible. The lymphatic damage will still be there, and you’ll need to keep up with self-care to prevent swelling from returning, but many people can live without noticeable swelling if they start treatment early enough.
Do you feel unwell with lymphedema?
You don’t feel sick with lymphedema, but you might feel discomfort, heaviness, or achiness in the affected area because of the swelling. If you suddenly feel sick, especially if you develop a fever, chills, or notice your swelling getting rapidly worse with redness and warmth, that’s a sign of infection that requires immediate medical attention and antibiotics.
What does breast lymphedema look like?
Breast cancer-related lymphedema in men typically shows up as swelling in the chest, arm, or shoulder on the side where you had surgery. The skin might look normal at first, but as lymphedema progresses, it can become stretched, shiny, or develop a pitted texture. Some men notice asymmetry, with one side of their chest or one arm being noticeably different from the other.
Does radiation therapy increase lymphedema risk?
Yes, radiation therapy to the chest or underarm area damages lymph vessels and increases your risk of developing lymphedema. Generally speaking, if you’ve had both lymph node surgery and radiation, your risk of developing lymphedema is higher than if you only had surgery.
Follow this breast cancer recovery roadmap to lower your lymphedema risk.
Prevent and Treat Lymphedema with Breast Cancer Rehab
As an oncology physical therapist and certified lymphedema therapist (CLT-LANA), my mission is to make lymphedema education and care more accessible to people everywhere.
In my practice, I often see people who’ve been living with lymphedema for many years before they’re able to access physical therapy or get guidance that goes beyond surface-level advice.
This problem is even worse for men who’ve had breast cancer. Because male breast cancer is rare, there’s less awareness, fewer resources, and less support available.
I also know that seeing a physical therapist in person isn’t realistic for everyone because of time constraints or cost. That’s why I created accessible and affordable resources that anyone with internet access can use.
Breast Cancer Rehab is my program for rehabilitation after breast cancer, and everything in it applies to men just as much as it does to women.
You can also use my digital guides with targeted exercises to support lymph drainage and manage your symptoms!